LITTLE ROCK — Arkansas stands to save $670 million over the next decade by extending private health insurance to about 250,000 low-income Arkansans through the state’s Medicaid program, according to a report released Wednesday by the state Department of Human Services.
In the final weeks of the legislative session, lawmakers are deciding whether to provide access to health coverage via private insurance, put those 250,000 people on the state Medicaid program or do nothing. The third option would leave people making between 17 percent and 100 percent of the federal poverty level, $4,244 to $11,170 for an individual, without financial help to get health insurance.
The session is scheduled to end April 19. Members are also considering $100 million in various tax cuts and an overhaul of the current $5 billion Medicaid program, which serves about 780,000 people - issues legislative leaders say need to be addressed in tandem.
The 2010 federal Patient Protection and AffordableCare Act let states choose to extend their state Medicaid program to cover those making up to 138 percent of the federal poverty line, or $15,145 annually for an individual.
In late February, Gov. Mike Beebe got federal approval for a “private option” to extend insurance coverage to those making up to the 138 percent level.
If the state chooses the private option route, the federal government will pay premiums for private companies to provide health-insurance coverage through the state’s private insurance exchange to an estimated 250,000 of the state’s poorest residents.
On March 18, draft legislation expanding that access circulated at the Capitol, but the language has not been added to a bill.
Members involved in daily negotiations over whether to move forward said the numbers may help make the case for the private option.
“It helps further the conversation. It supports some of the assumptions that we were making in developing the plan,” Sen. Jonathan Dismang, R-Beebe, said.
Dismang said he is speaking with House and Senate leaders about when to begin pushing legislation.
“I would assume sometime very quickly; I’m not sure the exact date on when that will drop,” Dismang said. “We are working with the goal of having something presented and voted on by the end of the session.”
Senate Democratic Leader Sen. Keith Ingram, D-West Memphis, said the numbers may resolve lingering questions and help bring the session to a close.
“We can’t take on tax cuts until we know the effect of Medicaid and the impact it’s going to have on the budget,” Ingram said.
“Obviously these numbers are very positive.”
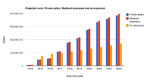
The report shows that between fiscal 2014, which begins July 1, and fiscal 2023, expanding access under the private option would have a $670 million impact on the state.
The benefits would come largely during fiscal 2015, 2016, and 2017, years when the federal government would pay 100 percent of the cost. The state would gradually take on a share of the cost until by 2020 it would be responsible for 10 percent.
The report shows expansion would have a positive effect of $151 million in fiscal 2015, $176 million in fiscal 2016 and $146 million in fiscal 2017. By fiscal 2021, expansion would cost the state less than$11 million a year.
Human Services Director John Selig said the totals come from a mix of reduced spending and more people paying taxes.
For example, the $151 million total for fiscal 2015 includes a $63 million bonusfor the state general revenue budget from spending $30 million less on Medicaid and $33 million less on uncompensated care. The rest includes $32 million from more people paying the tax on insurance premiums - because more people will have insurance - and $57 million in other tax revenue from federal tax dollars coming into the state.
The report also addressed concerns that having the federal government pay for private insurance would cost 50 percent more than providing access through Medicaid, as estimated last year by the Congressional Budget Office. State officials have said that number is based on nationwide figures and were not Arkansas specific.
“The federal cost will actually be less under this proposed private option then they would have been if we do the standard Medicaid approach that other states have taken,” Selig said.
According to the report, over 10 years the federal government will pay $592 million less if the state agrees to the private option.
Some legislators said they were skeptical of the numbers, in part because about a year ago the state Medicaid program was warning of a shortfall of as much as $400 million. That number has been revised repeatedly, and program officials now estimate that the projected $61 million shortfall will be resolved by expansion.
“At first glance, I’m confused,” House Democratic Leader Rep. Greg Leding, D-Fayetteville, said.
The study was done by Optumas, a nationally recognized actuarial consulting company, Selig said.
“You have to go with somebody’s estimates and these are best people we know to give us estimates And they are not far off from the estimates that were made here in the state,” Selig said. “I’d say you can trust these numbers.”
Optumas is a subcontractor hired by Manatt, Phelps and Phillip LLP, which has a $1.2 million federally funded contract with the Insurance Department to help Arkansas define the expansion options available, recommend which is best for the state and help Arkansas put it in place.
The contract ends Sept. 30.
A separate report released Tuesday by the Society of Actuaries found that medical claims costs in Arkansas will raise by an estimated 41 percent. The claims cost is what will be borne by insurance companies.
The report’s findings assume all 50 states will expand access to the traditional Medicaid program.
Several states have already announced they will not ex-pand Medicaid. The report does not include the private option.
Tennessee Gov. Bill Haslam announced Wednesday that he won’t expand the state’s Medicaid program to 140,000 uninsured Tennesseans after negotiations with the federal government broke down.
Even if no state expands Medicaid, Arkansas’ claims cost would increase by 40.4 percent, it states.
The report estimates that states such as Ohio and Wisconsin would see their claims cost increase by 80 percent or more. States such as Massachusetts, New York and Vermont would see a double digit drop in claims cost.
Front Section, Pages 1 on 03/28/2013