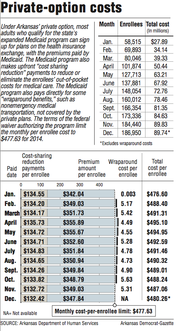
The average per-person payments to insurance companies under Arkansas' private-option Medicaid program fell this month for the eighth consecutive month, according to figures released Thursday by the state Department of Human Services.
The state Medicaid program this month paid the insurance companies $89.8 million on behalf of 186,950 Arkansans who were enrolled in health plans as of Nov. 15, the figures show.
That was an average payment per person of $480.26, a drop of $1.49 compared with the average payment last month.
After peaking at $490.61 in April, the per-person payments to insurance companies have fallen every month.
But the average cost, which includes the cost of providing certain services not covered by the private plans, remains above a target of $477.63 set in a federal waiver authorizing the program.
Including the cost of providing "wraparound benefits," the average total monthly cost of the private option from January through November was $489.98 per enrollee.
Human Services Department officials have attributed the higher-than-expected costs to an average age of enrollees that has been older than predicted. The costs have fallen as younger people have enrolled, officials have said.
At a meeting Thursday of the House and Senate public health committees, Human Services Department Director John Selig reiterated that he expects next year's costs to be well below the target of $500.18.
The department had predicted that costs would rise an average of 4.7 percent per year, but next year's premiums will be flat compared with this year, he said.
"We will save so much next year that it will more than compensate for what we're over this year," Selig said.
Sen. David Sanders, R-Little Rock and a sponsor of the law creating the private option, has said he expects the costs for 2014 to be reduced by requirements that insurance companies refund money to the Medicaid program if their spending on enrollees' medical care ends up being lower than the companies projected.
"The carriers have already told us they anticipate giving money back to the state," Sanders said Thursday.
Under the terms of the waiver, the federal government will pay the full cost of the private option through 2016, as long as the state's per-enrollee spending for the three years is below the cap that will be calculated using the monthly per enrollee targets.
In 2016, the monthly target rises to $523.58. If the state's costs are above the cap, it will owe the difference to the federal government.
Arkansas created the private option as a primary way to extend Medicaid coverage to adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Most of those made eligible by the expansion receive the coverage through insurance plans sold on Arkansas' insurance exchange, with the Medicaid program paying the premium and providing additional subsidies, known as cost-sharing reduction payments, to reduce or eliminate enrollees' out-of-pocket spending for medical care.
Those who are determined to have exceptional health needs -- about 10 percent of those made eligible by the expansion -- are covered under the traditional, fee-for-service Medicaid program.
This month's average premium payment to the carriers was $347.84, a drop of $1.19 compared with the average premium payment for November.
The average cost-sharing reduction payment fell by 31 cents, to $132.42.
The figures released Thursday also show the per-enrollee cost of nonemergency medical transportation and wraparound benefits fell to $5.31 in November, compared with $5.63 in October.
The cost of providing the wraparound benefits for December hasn't been determined.
The cost figures released by the Human Services Department were slightly revised from those released last month.
Special language passed by the state Legislature this year to reauthorize the private option requires the Human Services Department to limit nonemergency transportation by private-option enrollees and to establish a program allowing them to create "independence accounts" by Feb. 1.
At Thursday's meeting of the public health committees, state Surgeon General Joe Thompson said officials hope to receive approval from the Centers for Medicare and Medicaid Services for the independence account program within the next few weeks.
The program would encourage enrollees with incomes greater than 50 percent of the poverty level to make monthly payments, ranging from $5 to $25, to help pay the cost of their medical care.
The state would provide a match of up to $15 for each enrollees' contribution, with the state match deposited in an account that could be used to pay a premium for a non-Medicaid insurance plan when the enrollee leaves the private option. The balance in the account would be capped at $200.
Enrollees who make a contribution for a given month would not have to pay out of pocket for their medical care for that month. Currently, enrollees with incomes above the poverty level have copayments for some services -- $8 for a doctor's office visit, for instance.
Thompson said the program is expected to start in January for enrollees with incomes above the poverty level, with the first payments by enrollees due in February.
Enrollees with incomes below the poverty level would begin making payments in June, he said. In the meantime, Little Rock-based Datapath, which is administering the program, will begin a campaign to educate enrollees about it.
The program's administrative costs will total about $15 million a year, with half of that amount coming from state funds and the rest coming from the federal government, Thompson said.
Also on Thursday, the public health committees reviewed the Human Services Department's plan to offer additional benefits to children covered under the ARKids First B health insurance program and add it to the state's Children's Health Insurance Program plan effective June 1.
The additional services -- inpatient psychiatric care, orthodontics and occupational, physical and speech therapy -- will cost the state about $2 million through Oct. 1, when the federal government will begin paying the full cost of the program, state Medicaid Director Dawn Stehle said.
The waiver authorizing ARKids B had been set to expire Dec. 31, but the Centers for Medicare and Medicaid Services granted a five-month extension after members of the public health committee complained in November that they hadn't been told about the change earlier.
Metro on 12/19/2014