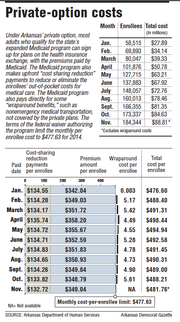
The average per-person payments to insurance companies under Arkansas' private-option Medicaid program fell this month for the seventh consecutive month, according to figures released Thursday by the state Department of Human Services.
The state Medicaid program on Nov. 13 paid the insurance companies $88.8 million on behalf of the 184,344 Arkansans who were enrolled in health plans as of Oct. 15, the figures show.
That was an average payment of $481.76 per person, down 84 cents from the average per-person payment last month.
After peaking at $493.95 in April, the per-person payments to insurance companies have fallen every month.
But the average cost, which includes the cost of providing certain services not covered by the private plans, remains above a target of $477.63 set in a federal waiver authorizing the program.
Including the cost of providing the so-called "wraparound benefits," the average total monthly cost of the private option from January through October was $490.69 per enrollee.
Human Services Department officials have attributed the higher-than-expected costs to an average age of enrollees that has been older than predicted.
But department Director John Selig has said that next year's monthly costs are expected to be well below the target of $500.18 for 2015 and will more than make up for this year's monthly average when the total cost of the program over its three-year demonstration period is calculated.
Under the terms of the waiver, the federal government will pay the full cost of the private option through 2016, as long as the state's per-enrollee spending for the three years is below the cap that will be calculated using the monthly per enrollee targets.
In 2016, the monthly target rises to $523.58. If the state's costs are above the cap, it will owe the difference to the federal government.
Sen. David Sanders, R-Little Rock, and a sponsor of the law creating the private option, said Thursday that the monthly cost figures are important but also represent just a "snapshot in time."
He reiterated that he expects the costs for 2014 to be reduced by requirements for insurance companies to refund money to the Medicaid program if their spending on enrollees' medical care ends up being lower than the companies projected.
Arkansas created the private option as a primary way to extend Medicaid coverage to adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Most of those made eligible by the expansion receive the coverage through insurance plans sold on Arkansas' insurance exchange, with the Medicaid program paying the premium and providing additional subsidies, known as cost-sharing reduction payments, to reduce or eliminate enrollees' out-of-pocket spending for medical care.
Those who are determined to have exceptional health needs -- about 10 percent of those made eligible by the expansion -- are covered under the traditional, fee-for-service Medicaid program.
This month's average premium payment to insurance companies was $349.04, up 25 cents from the average premium payment for October. That was the first time the average premium had increased since April.
But the average cost-sharing reduction payment fell by $1.09, to $132.72, leading to the overall drop in the average payment.
Human Services Department spokesman Amy Webb has said that the average premium has generally fallen as younger people have enrolled. The drop over several months in the average cost-sharing reduction payment appears to be the result of higher enrollment by people with incomes above the poverty level, Webb has said.
The cost-sharing reduction payment for those enrollees is lower because the enrollee is required to make some co-payments -- $8 for a doctor's office visit, for instance.
Webb said she didn't have information Thursday on what led to this month's increase in average premium.
The figures released Thursday also show that the per-enrollee cost of nonemergency medical transportation and other so-called "wraparound benefits" not covered by the private plans increased from $4.90 in September to $5.61 in October. That figure for November was not yet available.
Webb said that rise was tied to an increase in the number of rides provided to traditional Medicaid recipients. The higher number of rides led to an increase in the "utilization factor" that's used to calculate the payment to transportation companies for beneficiaries of the traditional Medicaid program as well as private-option enrollees, Webb said.
The cost for private-option enrollees is expected to fall when new contracts with the transportation companies take effect on July 1, Webb said. Those contracts will have separate rates for private-option enrollees and recipients of the traditional Medicaid program, she said.
Metro on 11/21/2014