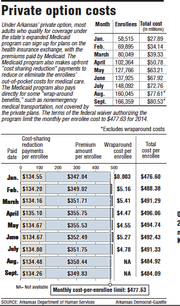
Correction: The average per-enrollee payment to insurance companies for coverage under the Arkansas’ private option Medicaid program peaked in April at $491.59, according to the state Department of Human Services. The Medicaid program also paid an average of $4.47 per enrollee that month for services not covered by the private plans, for a total per-enrollee cost of $496.06. A story in Friday’s newspaper about the cost of the program listed an incorrect figure for the average per-enrollee payment to the insurance companies for April.
The per-person premium for Arkansans enrolled in the so-called private option Medicaid program fell for the fifth month in a row as younger people continued to enroll in the program, a spokesman for the Arkansas Department of Human Services said Thursday.
The state Medicaid program made monthly payments to insurance companies on Thursday totaling $80.5 million on behalf of 166,359 enrollees for coverage this month, department spokesman Amy Webb said.
That was an average of $484.09 per enrollee, a decrease of 83 cents compared with the average per-enrollee payment for coverage in August.
A federal waiver authorizing the private option sets a target for the monthly per-enrollee cost of the private option at $477.63.
Medicaid officials have said that the costs have exceeded projections because the average age of enrollees has been older than predicted, resulting in higher premiums.
But the per-person payments have fallen each month after peaking in April at $496.06.
"As we said previously, we thought the age peaked a couple months ago, and we expected it to continue to go down," Webb said.
The terms of the waiver from the U.S. Department of Health and Human Services' Centers for Medicare and Medicaid Services allow the annual target to be adjusted if the state has information that the target "may underestimate the actual costs of medical assistance for the new adult group."
Webb reiterated Thursday that Medicaid officials don't plan to request an adjustment in the target for 2014.
"We still have an opportunity to revisit that if we need to," she said.
The deadline to request an adjustment is Oct. 1.
Under the private option, most people who qualify for coverage under the state's expanded Medicaid program receive the coverage through plans sold on the state's health insurance exchange, with the Medicaid program paying the premiums.
Those who are determined to have exceptional health needs are covered under the traditional, fee-for-service Medicaid program.
The expansion approved by the Legislature last year extended eligibility to adults with incomes of up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Enrollment began in October for coverage that started in January.
The fee-for-service Medicaid program covers the medical expenses of those in the private option until their coverage under the private-option plan kicks in.
The payment to insurance companies for this month is for coverage for those who had completed enrollment as of Aug. 15.
In addition to premiums, the payments to insurance companies include subsidies that reduce or eliminate enrollees' out-of-pocket spending for medical care.
The Medicaid program also pays directly for some "wraparound" services, such as nonemergency medical transportation, required by federal Medicaid rules but not covered by the insurance plans.
Through July, the monthly wraparound costs have averaged $4.51 per enrollee.
During the same period, the total monthly costs per enrollee, including the wraparound costs, averaged $491.33.
Information on the wraparound costs for August wasn't available Thursday.
Under the terms of the private-option waiver, the federal government will pay the full cost of the program through 2016, as long as the state's per-enrollee spending for the three years is below a cap, which will be calculated using the monthly per-enrollee targets. The cost of the wraparound coverage will be included in the calculation of the program's cost.
The monthly target used to calculate the cap rises to $500.08 in 2015 and $523.58 in 2016.
Webb has said Medicaid officials expect this year's costs to be reduced by a provision in the 2010 federal health care law requiring insurance companies to issue refunds if they spend less than 80 percent of the premiums they collect on medical care, rather than administrative expenses or profits.
In the case of the private option, any refunds issued would go to the Medicaid program, offsetting the private option's cost.
If the companies' expenses for enrollees' medical care are below projections, the companies could also have to refund some of the upfront payments they received to reduce enrollees' deductibles and copayments, Webb noted.
Max Greenwood, a spokesman for Arkansas Blue Cross and Blue Shield, said Thursday that her company and the national Blue Cross and Blue Shield Association don't anticipate owing any money to the Medicaid program.
Representatives of Little Rock-based QualChoice Health Insurance and St. Louis-based Centene Corp., which are also offering plans on the state's health insurance exchange, said last month that it was too early to say how spending on enrollees' medical care will compare with projections. The company representatives didn't return calls seeking comment Thursday afternoon.
The figures for the payment total in April and wraparound costs for February through June have been revised slightly since the Human Services Department originally released them.
For instance, the Human Services Department reported in April that the average per-enrollee payment to insurers for that month was $490.85 .
The revised wraparound costs are slightly lower than what the Human Services Department originally reported. For instance, the wraparound-cost total for June was originally reported to be $731,801.74. The report to the Legislature's public health committees listed the June cost as $727,107.37.
Webb said she didn't have information Thursday on why the figures were revised.
A Section on 09/12/2014