The average per-person payment to insurance companies for coverage under Arkansas' private option fell by about 4 cents this month to its lowest level since January, a spokesman for the Arkansas Department of Human Services said Tuesday.
The Human Services Department on April 9 paid the companies $101,070,565.75 on behalf of 209,896 Arkansans who had completed enrollment as of March 15, department spokesman Amy Webb said in an email.
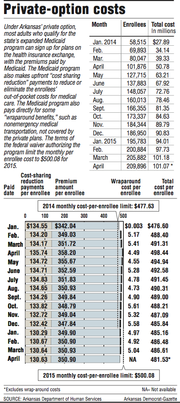
That was an average payment of $481.53 per enrollee. The average payment was $481.57 in March, $481.56 in February and $480.18 in January.
Information released Tuesday also shows that, including the cost of nonemergency transportation and other benefits paid for directly by the traditional Medicaid program, the monthly cost of the private option averaged $486.09 per enrollee from January through March.
That cost is $3.61 below the average per-enrollee cost of the program in 2014 and $13.99 below the target for 2015 in the federal waiver authorizing the program.
The federal government will pay the full cost of the program through 2016 as long as the cost over three years is below a cap that will be calculated using such monthly cost targets.
If Arkansas' costs exceed the cap, the state will owe the difference to the federal government.
A legislative task force will take the cost of the private option into account as it researches alternatives to the program, Sen. Jim Hendren, R-Sulphur Springs and a co-chairman of the panel, said Tuesday.
He added that the task force will be studying ways of providing coverage to all Arkansans now covered by Medicaid, including those in the traditional Medicaid program.
About 700,000 Arkansans, including low-income children, elderly and disabled people, were covered by the traditional Medicaid program as of Sept. 30.
"My expectation is that the data is going to show that even with us being below the caps, there are more affordable and economical ways to deliver health care services to people than private insurance policies for the entire population," Hendren said.
Arkansas created the private option in 2013 as a primary way to expand Medicaid coverage as authorized under the federal Patient Protection and Affordable Care Act of 2010.
The program uses Medicaid funds to buy coverage on the state's health insurance exchange for adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Adults who are deemed to have exceptional health needs, making up about 10 percent of those made eligible under the expansion, are covered under the traditional, fee-for-service Medicaid program.
Last year, the monthly cost of the private option averaged $489.70 per enrollee -- more than $12 above the waiver's target of $477.63 for 2014.
The target rose this year to $500.08. Next year, it will rise to $523.58.
The payment for this month was composed of an average monthly premium of $350.90 and an average of $130.63 in subsidies, known as cost-sharing reduction payments, that are meant to reduce or eliminate enrollees' out-of-pocket expenses for medical care.
The premiums vary according to the plan selected by the enrollee and the enrollee's age. The companies charge higher premiums to insure older enrollees.
Cost-sharing reduction payments are lower for enrollees with incomes above the poverty level because they are required to make some co-payments -- $8 for a doctor's office visit, for instance -- or contribute up to $15 per month to help pay the cost of their medical care.
Compared with the payments for March, the average premium was about 3 cents lower for April, and the average cost-sharing reduction payment was about 1 cent lower.
In addition to the payments to insurance companies, the Medicaid program pays directly for nonemergency medical transportation and other benefits that are required to be provided under Medicaid rules but aren't covered by the insurance companies' plans.
The cost of those so-called wraparound benefits averaged $5.04 per enrollee in March, compared with $4.92 in February and $4.97 in January.
During all of 2014, the monthly cost of the wraparound benefits averaged $4.91 per enrollee.
Even if Arkansas' costs are below the cap, the state will be responsible for 5 percent of the cost of covering the expanded Medicaid population in 2017. The state's share will then rise each year until it reaches 10 percent in 2020.
Citing concerns about the cost and opposition from legislators and others, Gov. Asa Hutchinson in January called on the Legislature to create the task force to recommend an alternative way of providing coverage after Dec. 31, 2016.
Six firms -- Salt Lake City-based Leavitt Partners; The Stephen Group of Manchester, N.H.; Lansing, Mich.-based Health Management Associates; Chicago-based Navigant Consulting; Seattle-based Milliman; and Boston-based Public Consulting Group -- submitted bids to provide consulting services to the task force before a deadline of 4:30 p.m. Friday, said Marty Garrity, director of the state Bureau of Legislative Research.
The task force is likely to select a firm during meetings next week.
Metro on 04/29/2015