A legislative task force plans to make recommendations today on changes to the state's Medicaid program, including changes to the private option and whether to hire managed-care companies to provide coverage for recipients with expensive medical needs.
Under the private option, the state uses Medicaid funds to buy coverage on the federally run insurance exchange for low-income adults.
The Legislature created the program in 2013 as a primary way to extend health coverage to adults with incomes of up to 138 percent of the poverty level: $16,243 for an individual, for instance, or $33,465 for a family of four.
According to information released by the state Department of Human Services this week, 249,539 Arkansans had been approved for coverage under the expanded program as of Nov. 30.
That included 198,917 Arkansans who completed enrollment in the private option as of Oct. 15 and 22,839 others who are covered under the traditional fee-for-service Medicaid program because their health needs are considered exceptional.
Thousands of others had been approved for coverage but had not yet completed enrollment.
Gov. Asa Hutchinson, who is expected to address the task force today, has called for a number of changes to be incorporated into a revamped private option that would be named Arkansas Works.
That includes requiring enrollees with incomes above the poverty level to pay premiums of up to 2 percent of their incomes and establishing "lockout" periods for those who fail to pay.
Hutchinson also has called for excluding or charging higher premiums to Arkansans who own significant assets, such as houses; subsidizing coverage through employer plans for those with access to job-based coverage; referring unemployed enrollees to job programs; strengthening procedures for verifying recipients' eligibility for benefits; and finding ways to reduce the expenditure of state tax dollars on Medicaid by at least $50 million a year.
At a conference of Medicaid providers last week, Hutchinson also expressed support for offering vision and dental benefits to certain enrollees to encourage work or healthful behavior and for charging premiums or copayments to enrollees with incomes below the poverty level.
Most of the proposed changes would require waivers from federal Medicaid rules.
Sen. Jim Hendren, a chairman of the task force, said he expects the panel's recommendations on the private option to help Hutchinson as he prepares to seek approval for the changes from federal officials.
"I think most people see the wisdom in at least continuing a dialogue and authorizing the governor to go negotiate based on the framework he's laid out there," Hendren, R-Sulphur Springs, said after a task force meeting Tuesday.
"There's going to be a fight coming on the Medicaid expansion, but it's not going to be until we know what it's going to look like," he said, "and we don't know that until the federal government tells us what they will or will not do."
In calling on the Legislature to create the task force earlier this year, Hutchinson cited some lawmakers' opposition to the private option and the eventual cost of the program to the state.
As long as the cost of the program stays below a cap based on monthly per-enrollee cost targets, the federal government is expected to pay the full cost of the private option until 2017, when Arkansas will be responsible for 5 percent of the cost.
The state's share of the private option will then increase every year until it reaches 10 percent in 2020.
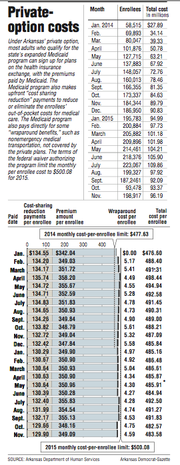
According to information released by the Human Services Department this week, the average per-enrollee cost of the private option rose by just over $1, to $483.58, in November after falling by more than $9 in October.
Since it started in 2014, the program's expenses totaled about $1.9 billion through November, about $16.9 million below the cap based on the monthly targets.
Despite opposition by some lawmakers to the private option, much of the debate within the task force has focused on whether to hire managed-care companies to provide benefits for recipients in the traditional Medicaid program as a way of reducing costs.
Under that approach, the companies would be paid a fixed amount per recipient and would be responsible for the recipients' care.
A consultant hired by the task force said in October that the state could save $2.4 billion in state and federal funds between 2017 and 2021 by hiring managed-care companies to pay for services for the entire traditional Medicaid program.
Over the same period, the state could save almost $2 billion by hiring such companies only for the high-cost recipients, according to the firm.
If the state implements its own payment changes without hiring managed-care companies, the state could save $708 million, the firm said in its report.
Hutchinson has said he supports using managed care for recipients with expensive medical needs while continuing with the state's own efforts to reduce the cost of care for others.
According to a draft summary of options prepared by The Stephen Group, Hutchinson supports managed care for the developmentally disabled and mentally ill.
Under a "carve out," the state would change how it pays nursing homes without placing them under managed care, according to the summary.
Hutchinson spokesman J.R. Davis said Tuesday evening that he didn't have details on Hutchinson's proposal for managed care.
At the task force meeting Tuesday, four members -- Reps. Michelle Gray, R-Melbourne, Justin Boyd, R-Fort Smith, Joe Farrer, R-Austin, and Deborah Ferguson, D-West Memphis -- and Sen. Missy Irvin, R-Mountain View, presented their own proposal, called DiamondCare.
Under their approach, the state would hire managed-care companies to provide dental benefits while implementing its own cost-cutting efforts in the rest of the program.
The Arkansas Foundation for Medical Care, a nonprofit organization, would help coordinate the care for the developmentally disabled and mentally ill.
"I think we can do it ourselves in the state of Arkansas better" than by hiring managed-care companies, Gray said.
A Section on 12/16/2015