More than 10,000 Arkansans were approved for coverage under Arkansas' expanded Medicaid program in December and January, bringing the total to 233,518, the state Department of Human Services reported Wednesday.
The department also reported that the average per-person payment to insurance companies under the program's private option, which covers most of the new enrollees, rose this month for the first time in 10 months.
Meanwhile, the U.S. Department of Health and Human Services reported that enrollment in coverage through the state's health insurance exchange among those who did not qualify for Medicaid rose to 64,947 as of 11 p.m. Sunday, up from 58,878 as of Feb. 6.
Nationwide, 11.4 million people were enrolled in non-Medicaid coverage through exchanges, Health and Human Services Secretary Sylvia Burwell said in a blog post.
"The Affordable Care Act is now an important part of the everyday lives of millions of Americans," Burwell said.
Arkansas created the private option as the state's primary way to expand Medicaid coverage to adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Those deemed to have exceptional health needs are covered under the traditional, fee-for-service Medicaid program.
Federal tax credit subsidies are available to many who don't qualify for Medicaid and have incomes below 400 percent of the poverty level: for example, $45,960 for an individual or $94,200 for a family of four.
Those covered under the expanded Medicaid program as of Jan. 31 included 195,520 who were enrolled in the private option, up from 188,083 who were enrolled as of Nov. 30, the state Human Services Department reported.
During the same period, the number who were assigned to the traditional Medicaid program because of their health needs dropped from 25,117 to 23,516.
An additional 14,482 Arkansans had been determined eligible for the private option but had not completed enrollment as of Jan. 31.
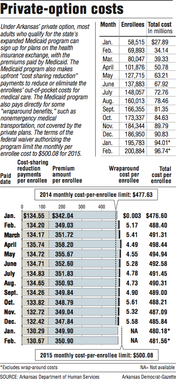
Arkansas' Feb. 12 payment to the insurance companies for coverage under the private option totaled $96.7 million on behalf of 200,884 Arkansans.
That was an average payment of $481.56 per enrollee, an increase of $1.38 compared with the average payment last month.
From January to this month, the average premium rose $1, to $350.90, while the average cost-sharing reduction payment rose 38 cents, to $130.67.
The monthly per-enrollee cost has been watched because of a cost cap, set in the federal waiver authorizing the private option, that will be calculated using monthly per-enrollee cost targets.
Last year, the monthly cost, including payments for nonemergency transportation and other services not covered by the private plans, averaged $489.70 per enrollee -- more than $12 above the 2014 target.
Human Services Department spokesman Amy Webb said she didn't know the reason for this month's increase in average premium, but she noted that the cost remains below the monthly target of $500.08 per enrollee for 2015.
Department officials expect the cost to remain well below the target this year, she said.
"We never expected just to continually see a decline every month," Webb said. The cost is "going to fluctuate, and that's OK."
Premiums, which are set by the insurance companies and approved by state and federal officials, vary according to the plan an enrollee selects and the enrollee's age, with higher premiums charged for older enrollees.
Human Services Department officials said last year's costs were higher than expected due to an average age of enrollees that was older than expected.
The cost fell as younger people enrolled, department officials said.
The program's cost also includes payments for services, such as those for nonemergency medical transportation, that Medicaid rules require to be covered but that aren't covered by the private plans.
During all of 2014, the cost of those so-called wraparound benefits averaged $4.91 per enrollee. Information on the wraparound costs for January wasn't available Wednesday.
Under the terms of the waiver issued by the U.S. Department of Health and Human Services' Centers for Medicare and Medicaid Services, the federal government will pay the full cost of the private option through 2016, as long as the state's spending is below the cap.
The monthly target for 2014 was $477.63. It will rise next year to $523.58.
If the state's costs are above the cap, it will owe the difference to the federal government.
Arkansas and other states that have expanded Medicaid will be required to pay 5 percent of the cost in 2017. Each state's share will then rise each year until it reaches 10 percent of the state's cost in 2020.
Citing opposition by some legislators and other Arkansans and a concern about the state's share of the cost, Gov. Asa Hutchinson has called for a legislative task force to recommend alternatives to the private option starting in 2017. He signed legislation last week creating the task force.
For those who don't qualify for Medicaid, the deadline to sign up for coverage through an insurance exchange for 2015 was 2 a.m. Monday. But many people who started applications before the deadline but didn't finish them are being given until Sunday to complete enrollment, Burwell said.
The extension is available to those who experienced longer-than-normal wait times to speak with an operator at a federal call center or who had technical difficulties with the federal enrollment portal, healthcare.gov.
Those who qualify for Medicaid can enroll at any time throughout the year but can change plans only during the annual enrollment periods.
Metro on 02/19/2015