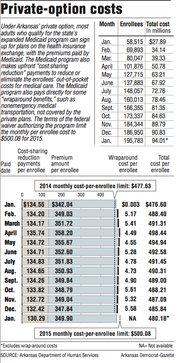
During the first year of Arkansas' private option, the program's monthly cost per enrollee averaged $489.70 -- more than $12 above the target set under the terms of a federal waiver, figures released Tuesday by the state Department of Human Services show.
But the figures also show that that average per-enrollee payment to insurance companies for January fell to $480.18, almost $20 lower than the target set in the waiver for 2015.
Department officials expect the cost of the program over three years to be below the limit set in the waiver from the U.S. Department of Health and Human Services' Centers for Medicare and Medicaid Services, Human Services Department spokesman Amy Webb said.
"We've made some adjustments in Year Two, and I think there are some additional tools we could utilize in Year Three if we saw there could be a concern," Webb said. "Right now, we don't think there will be concern."
Sen. David Sanders, R-Little Rock, and a sponsor of the law creating the private option, said the cost for January is "a positive sign that the program is working."
"We are, in real time, proving what had been the unprovable fact, and that is that with a large-scale premium assistance model, even with all the regulatory framework that we face and the hurdles that we face, we can see declines in the cost," Sanders said.
He said he still expects the costs for last year to be lowered by requirements that insurance companies refund money to the Medicaid program if their spending on participants' medical care ends up being lower than the companies projected.
Senate Republican leader Jim Hendren of Sulphur Springs, who is sponsoring a bill that would create a task force to study alternatives to the private option, said the falling cost is "good news" but doesn't satisfy his concerns.
"Those of us that did not favor expanding Medicaid did so because the long-term cost on the state budget is going to be dramatic," Hendren said.
Arkansas created the private option as the state's primary way to expand Medicaid coverage to adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
Most of those made eligible by the expansion receive the coverage through insurance plans sold on Arkansas' insurance exchange, with the Medicaid program paying the premium and providing additional subsidies, known as cost-sharing reduction payments, to reduce or eliminate enrollees' out-of-pocket spending for medical care.
Those who the state determines to have exceptional health needs -- about 10 percent of those made eligible by the expansion -- are covered under the traditional, fee-for-service Medicaid program.
In 2013 and 2014, legislators narrowly approved funding for the program by the three-fourths majority required for appropriation bills.
Gov. Asa Hutchinson last week proposed continuing funding for the program through 2016 and appointing a legislative task force to study other ways to provide coverage to participants.
State Rep. David Meeks, R-Conway, who opposed Medicaid expansion, said Tuesday that he supports Hutchinson's plan.
"I think we can do things better than what we have now," he said.
The Human Services Department payments to insurance companies on Jan. 8 totaled more than $94 million on behalf of 195,783 Arkansans who had completed enrollment by mid-December.
The payments included an average monthly premium of $349.90, an increase of $2.06 compared with the average premium payment for December.
The average cost-sharing reduction payment was $130.29, a decrease of $2.13 compared with the average cost-sharing payment for December.
The net result was a drop of about 7 cents in the average payment per enrollee, from $480.26 for December to $480.18 for January.
After peaking at more than $490 in April, the average per-enrollee payment to insurance companies has fallen every month.
The program's cost also includes payments for services, such as nonemergency medical transportation, that Medicaid rules require to be covered but that aren't covered by the private plans.
The cost of providing such "wraparound" benefits in December was $5.58 per enrollee, compared with $5.32 for November. During all of 2014, the cost of the wraparound benefits averaged $4.91 per enrollee.
Under the terms of the waiver issued by the U.S. Department of Health and Human Services' Centers for Medicare and Medicaid Services, the federal government will pay the full cost of the private option through 2016, as long as the state's spending is below a cap, which will be calculated using monthly, per-enrollee cost targets.
The monthly target for 2014 was $477.63. It rose to $500.08 this year and will rise again next year to $523.58.
If the state's costs are above the cap, it will owe the difference to the federal government.
Even if the cost of the private option is below the cap, Arkansas will be required to pay 5 percent of the cost of providing coverage to the newly eligible enrollees in 2017. The state's share will then rise every year until it reaches 10 percent in 2020.
State Human Services Department officials have said the cost of the private option for 2014 was higher than expected because the average age of participants was older than expected, leading to higher premiums.
The average premium fell as younger people enrolled.
To hold down costs this year, state officials specified that the plans covering private-option enrollees can cover only the benefits required by state and federal laws.
Those benefits do not include adult dental and vision coverage, which had been included in some plans offered last year by St. Louis-based Centene Corp.
Premiums for the private-option plans are essentially flat this year compared with last year, state Insurance Department officials have said. Overall, premiums for plans on the state's insurance exchange are an estimated 2.2 percent lower than last year, the officials have said.
A Section on 01/28/2015