As lawmakers explore possible changes to Arkansas' Medicaid program, one focus should be the care provided to the elderly, the disabled and people with mental illness, consultants told an advisory panel Thursday.
Compared with other states, Arkansas provides more care in institutional settings such as nursing homes instead of in people's homes or community settings, John Stephen, managing partner with The Stephen Group of Manchester, N.H., said at a meeting of the Governor's Advisory Council on Medicaid Reform.
And he noted that nursing-home staff members conduct assessments that are used to determine the type and level of care a Medicaid recipient needs.
"Your front door can't be driven and controlled and directed by providers," Stephen said. "Your front door has to be accountable to taxpayers as well as the program. It is not today."
The 40-member council, made up of state officials and representatives of the health care industry and advocacy groups, was appointed by Gov. Asa Hutchinson earlier this year to help develop recommendations for improving the state's Medicaid program.
The council is expected to provide input to a 16-member legislative task force that will make recommendations by the end of this year.
Those recommendations will include a replacement program for the state's so-called private option, which uses Medicaid funds to buy commercial insurance coverage for low-income Arkansans who became eligible for assistance last year under the expansion of the Medicaid program.
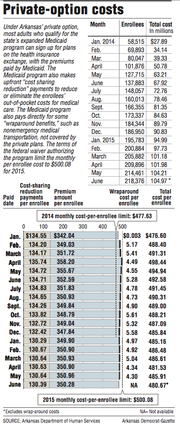
The state Department of Human Services reported Thursday that the number of newly eligible Arkansans approved for coverage grew in May by almost 4,000 people, to 254,749.
Meanwhile, the average per-enrollee payment to insurance companies for coverage under the private option fell in June by 94 cents, from $481.61 to $480.67.
As long as Arkansas' per-enrollee cost stays below a limit set in a waiver authorizing the private option, which was established under the federal Patient Protection and Affordable Care Act, the federal government is expected to pay the full cost of covering the private option through the end of 2016.
But Hutchinson has cited the eventual cost of the program to the state as a reason to replace it starting in 2017, when Arkansas will begin paying 5 percent of the cost of covering the newly eligible adults.
After 2017, the state's share will increase every year until it reaches 10 percent in 2020.
Citing figures from the Kaiser Family Foundation, Stephen said that about 34 percent of Arkansas' Medicaid spending in 2013 was on long-term care, compared with 28 percent of Medicaid spending nationally.
According to The Stephen Group's report last month to the Health Reform Legislative Task Force, almost 70 percent of the state's long-term-care spending is on nursing homes, with the rest going to assisted-living facilities and for home and community-based services.
The average cost per day of caring for a nursing-home resident averaged more than $140 per day in September 2014, compared with $63 per day for those in assisted-living facilities, according to the report.
That month, 13,275 Medicaid recipients were in nursing homes, compared with 749 who were in assisted-living facilities.
Residents of assisted-living facilities generally require less medical care than those in nursing homes but receive help with daily tasks, such as dressing and bathing.
"If you look at your balance sheet, and you compare it to other states, it's a significant issue," Stephen said. "You've got to work toward, in our opinion, a more robust community-based structure."
While nursing homes conduct assessments of their own prospective residents, state Human Services Department nurses assess Medicaid recipients' need for home- and community-based services, department spokesman Amy Webb said.
In 2011, the department hired CH Mack to develop an electronic tool to assess patients with developmental disabilities, but the company failed to develop a usable product, department officials have said.
After paying CH Mack $4.8 million, the department dropped the company last year and shifted the work to CoCENTRIX, which the department expects to pay $16.4 million over five years.
Department Director John Selig said his agency hopes to eventually conduct independent assessments, using a single tool, to determine Medicaid recipients' needs for a variety of long-term services, including nursing-home care.
The department has been "negotiating and working with providers and advocates about exactly how we implement it," he said, adding that implementing a new system would also require legislative review.
Arkansas' total Medicaid budget for the fiscal year that ended Tuesday was about $5 billion, with about 77 percent of the funds coming from the federal government.
Excluding expenditures on those who became eligible under Medicaid expansion, growth of the state's Medicaid spending has been about 2 percent annually in recent years, compared with growth rates as high as 8 percent to 10 percent in earlier years, Stephen said.
But the slowdown is typical of what states around the country have experienced, he said.
The state recovered $2 million in improper Medicaid payments last year, which he described as small compared with the state's overall Medicaid budget.
To make the program easier to manage, he said, officials should consolidate its nine federal waivers into a single "global waiver."
Arkansas' program "really isn't sustainable in its [current] form," said Stephen, the Stephen Group partner. "There are a number of areas that, in the future, you're going to be looking at, potentially going back to the taxpayers if you don't do it the right way."
Selig said the department is working with the inspector general for the state's Medicaid program on how to increase the recovery of improper payments.
"We agree completely that we could do more there," he said.
A Section on 07/03/2015