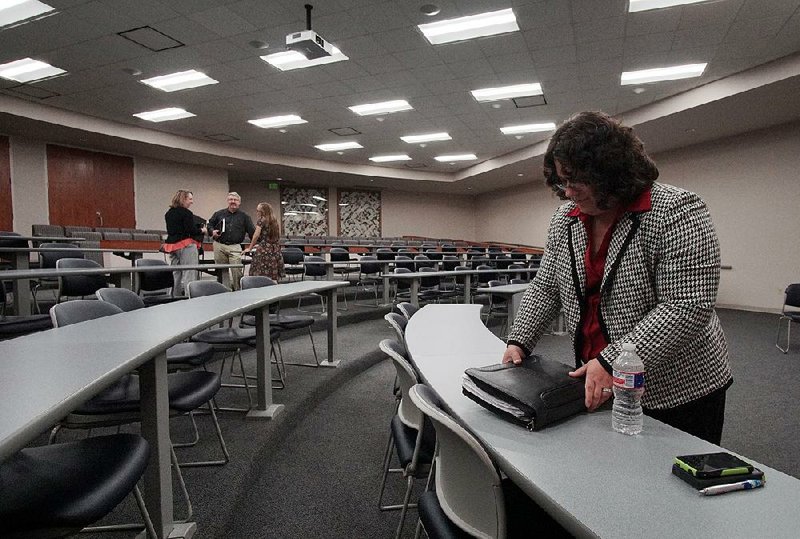
No one commented Thursday at a public hearing in Little Rock on Arkansas' plan to seek federal approval to make changes to the private option and extend the waiver authorizing it through 2021.
The changes, proposed by Gov. Asa Hutchinson and endorsed by the Legislature in a special session last month, include:
• Charging premiums of up to $19 a month to enrollees with incomes above the poverty level.
• Providing coverage to some enrollees through subsidized employer plans.
• Offering an extra benefit, such as dental coverage, as an incentive for enrollees to pay premiums and receive annual wellness exams.
The revamped program, now known as the Health Care Independence Program, would be renamed Arkansas Works when the changes take effect Jan. 1.
The state Department of Human Services released a draft of the waiver extension request May 18. It can be found on the state Medicaid website at medicaid.state.ar.us.
Amy Webb, a department spokesman, said the agency hadn't received any written comments on the proposal as of Thursday morning.
The department will continue to accept written comments through midnight June 17 and will hold a second public hearing at 5:30 p.m. Wednesday at Jefferson Regional Medical Center in Pine Bluff.
Written comments can be emailed to hciw@arkansas.gov or mailed to Division of Medical Services, Program Development and Quality Assurance, P.O. Box 1437, S-295, Little Rock, Ark. 72203-1437.
Under the private option, the state uses Medicaid funds to buy health coverage for low-income Arkansans through the state's federally run insurance exchange.
The state created the program in 2013 as a primary way to extend Medicaid coverage to adults with incomes of up to 138 percent of the federal poverty level: $16,394 for an individual, for instance, or $33,534 for a family of four. Almost 268,000 Arkansans were covered under the expansion as of Jan. 31.
The federal government has paid the full cost of Medicaid expansion -- about $1.6 billion annually -- since the coverage began in 2014. Starting next year, Arkansas will be responsible for paying 5 percent. The state's share will then rise each year until it reaches 10 percent in 2020.
Metro on 05/27/2016