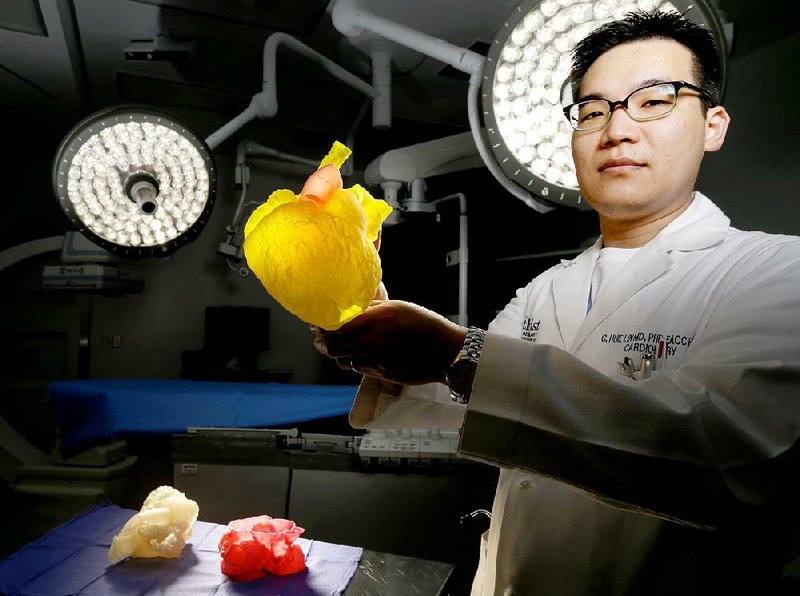
HOUSTON -- The yellow and pink heart in Dr. C. Huie Lin's office is an exact replica of the one beating inside the chest of Allison Bennie -- a 3-D model that helped save her life.
Two years ago, the 29-year-old South Carolina woman went to Lin, an interventional cardiologist at Houston Methodist Hospital, after being turned down for surgery elsewhere.
Lin is an expert in treating patients like Bennie, adults born with heart defects who, decades later, have outgrown the surgical repairs that saved them as infants. Adults with congenital heart defects tend to be complex cases, requiring specially tailored treatment, but Bennie's case came with an extra challenge: She's a Jehovah's Witness, a faith that forbids blood transfusions, even in surgery.
"Essentially," Lin said, "we needed to come up with a new way to fix the problem."
He had some ideas for how to repair her leaking pulmonary valve while minimizing blood loss, but to Lin's knowledge, none had ever been attempted on a patient with a congenital heart defect, and he couldn't be sure any would work.
"For me," Lin said, "this is where the story gets exciting."
Lin ordered a detailed scan of Bennie's chest and got in touch with William Dore Jr., a frequent Methodist donor and owner of 3DPrintLabs.com, a 3-D printing startup based in Houston. Dore agreed to print a $1,500 model of Bennie's heart at no cost and delivered it to the hospital.
"With this," Lin said, holding the heart model, "we could test out a solution that's never been tried before but without putting the patient needlessly at risk."
In Houston, and across the country, physicians are increasingly turning to 3-D printed organs to test complex operations, mostly relying on donations and grants to pay for the emerging technology. Dore and his company have printed defective hearts for Methodist, the brains of cancer patients for MD Anderson and earlier this year, the entire chest cavity of a child being treated for a rare defect at Texas Children's Hospital.
Dore is betting that his donations, and the work of physicians like Lin, will eventually prove the benefit of 3-D models in medicine and someday lead insurance companies to pay for them.
"In the cases we've done, there's been a tremendous cost savings in terms of minimizing complications and shorter recovery times," Dore said. "But in medicine, it just takes a long time for new ideas to become standard."
Lin has requested 3-D heart models for about a half-dozen patients, including Bennie, and eventually hopes to launch a clinical trial to test and prove their effectiveness.
"Adult congenital heart patients are the perfect group to test this out, because every patient is unique and requires personalized care," Lin said.
Bennie was surprised when she sat down with Lin and he showed her the model of her heart. It was amazing to hold it, she said. It was an exact copy of the organ that had kept her alive 27 years -- and caused her so many problems along the way.
She'd been born with a pulmonary valve so narrow, her tiny heart was straining to push blood through. A classic case of what's known as blue baby syndrome.
She went to Houston then, too. Dr. Denton Cooley, the legendary heart surgeon, opened her chest in 1988 and artificially enlarged the valve. But, like thousands of other infants saved by Cooley's scalpel, the repair came with a cost that wouldn't become apparent until decades later: The valve, now large enough for sufficient blood flow, was also made leaky and inefficient.
By 2015, Bennie had begun feeling fatigued. She couldn't catch her breath. Once again, her heart was straining, putting her at risk for heart failure. And once again, doctors back home told her they couldn't help and instead sent her to a specialist in Houston.
Before she arrived, Lin's team took the model of Bennie's heart into a lab at Methodist and tested his first idea: He wanted to use a catheter to pass a stent though an artery and into the valve and then inflate a balloon to deploy the stent, repairing the leak.
But when they attempted the procedure on the model, Lin realized immediately it wouldn't work. Bennie's pulmonary valve was so enlarged, the balloon couldn't deploy a stent large enough to stay in place.
"We knew that wasn't going to work," Lin said. "We needed to go another route."
Next, Lin and his team tested a procedure he's dubbed the hybrid approach, combining the initial catheter-based procedure with a surgical operation that would still minimize blood loss and avoid the need for a transfusion.
Before Lin snaked the stent and balloon through an artery, a surgeon would first open Bennie's chest and use a felt band to cinch down the valve, making it narrow enough to hold the stent in place. Bennie's heart would continue beating through the operation, avoiding the need to connect her to a heart-lung machine to pump blood through her body.
The medical team attempted the approach on the 3-D model, "and the stent deployed perfectly," Lin said.
To Lin's knowledge, the procedure had never been attempted before. But when he and the surgical team performed the operation on Bennie days later, they operated with confidence.
Two years later, she's doing well, she said. She was glad to learn Lin has held onto the model of her heart, a reminder of how hard doctors here worked to help her.
"It was comforting to know," Bennie said, "how much thought and effort they put into the operation."
SundayMonday Business on 04/24/2017