Two years after Arkansas expanded its Medicaid program, the state's residents were less likely to spend large amounts of their income on medical bills or go without care because of the cost, a report found.
The report by The Commonwealth Fund, a health policy research organization based in New York City, ranked Arkansas No. 36 among the states in the amount of access its residents had to health care services in 2016, up from No. 47 in 2013.
But in another report, by the United Health Foundation, a charity established by Minnetonka, Minn.-based UnitedHealth Group, Arkansas continued to rank No. 48 in the overall health of its residents.
Even after Medicaid expansion took effect in 2014, the state's rates of obesity, diabetes, and deaths from heart disease and cancer continued climbing, that report found.
Joe Thompson, director of the Arkansas Center for Health Improvement, said such indicators reflect factors, including poor diet and a lack of exercise, that having coverage doesn't necessarily change.
"The health care system is really not going to achieve health," Thompson said. That's "going to take community and family behavioral change and investment."
Arkansas' Medicaid expansion, known as Arkansas Works, extended eligibility to adults with incomes of up to 138 percent of the poverty level. This year, that threshold is $16,643 for an individual or $33,948 for a family of four.
Under the so-called private option, most of those enrolled in the program receive the coverage through private insurance plans, with the state using Medicaid funds to pay most or all of the premiums.
To lower the cost of the program for the state, Gov. Asa Hutchinson has proposed lowering the income cutoff for eligibility to the poverty level and imposing a work requirement on those who remain on the program. As of last week, there had been no announcement of whether the federal government will approve the state's request to implement the changes.
The same year the expansion took effect, the 2010 Patient Protection and Affordable Care Act made tax subsidies for health coverage available to many people who don't qualify for Medicaid and who have incomes of up to 400 percent of the poverty level: $48,240 for an individual or $98,400 for a family of four.
Since then, the percentage of non-elderly Arkansans who lack insurance has fallen by more than half, from 19 percent in 2013 to 9 percent in 2016, according to figures from the U.S. Census Bureau's American Community Survey. The survey was cited in The Commonwealth Fund report, released earlier this month.
Citing data from a Centers for Disease Control and Prevention survey, The Commonwealth Fund report also found a decline in the number of "at risk" adults who reported that they had not seen doctors in two years.
"At risk" was defined as adults age 50 and over as well as younger adults who reported that they are in fair or poor health; have had a heart attack or stroke; or have ever been diagnosed with diabetes, high blood sugar, heart disease or asthma.
The percentage of such Arkansans who had not seen doctors fell from 18 percent in 2013 and 2014, to 15 percent in 2015 and to 13 percent in 2016, according to the report.
Similarly, the percentage of Arkansas adults who had not seen dentists in the past year fell from 19 percent in 2012 to 18 percent in 2014 and 16 percent in 2016. (The CDC includes the question about dental coverage in its survey every other year.)
Citing figures from the Census Bureau's Current Population Survey, the report also found a drop in the percentage of non-elderly Arkansans who spent a large amount of their incomes on medical bills.
That amount, for medical expenses excluding premiums, was defined as 5 percent or more of the annual income for households with incomes below 200 percent of the poverty level, or at least 10 percent of a household's income for those with higher incomes.
From 2015-16, the report found, an average of 18 percent of non-elderly Arkansans spent a large portion of their incomes on medical bills, down from an average of 21 percent in 2013 and 2014.
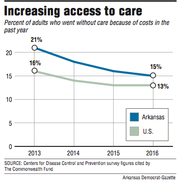
The percentage of Arkansas adults who went without care because of its cost fell three years in a row, from 21 percent in 2013 to 18 percent in 2014, 16 percent in 2015 and 15 percent in 2016, according to CDC survey data cited in the report.
In the United Health Foundation's annual report, also released this month, Arkansas' ranking in overall health improved from 49th to 48th in 2015 but hasn't budged since then.
The report calculates a health score for each state based on more than two dozen measures from a variety of sources.
In the latest report, Arkansas scored better than only Mississippi, which ranked last, and Louisiana.
Some of the measures indicate worsening health in Arkansas and other states.
In 2016, for instance, 35.7 percent of Arkansas' adults reported a height and weight indicating they are obese, up from 34.5 percent a year earlier.
Nationally, just under 30 percent of adults were obese in 2015 and 2016.
Meanwhile, 13.5 percent of Arkansas adults reported in 2016 that they have diabetes, up from 12.6 percent in 2015 and 11.5 percent in 2013.
Nationally, 10.5 percent of adults reported having diabetes in 2016, up from 9.9 percent in 2015 and 9.6 percent in 2013.
Arkansas had a higher rate of deaths from cardiovascular disease, including heart disease and stroke, and from cancer than all but three other states.
Using death rates adjusted to account for changes in the number of old and young people in the population, the report found that from 2013-15, Arkansas had an average of 323 deaths per year from cardiovascular disease per 100,000 residents, up from an average of 313.4 such deaths a year per 100,000 residents from 2011-13.
The age-adjusted death rate from cancer climbed from an average of 216.9 per 100,000 residents annually from 2011-13 to 219.5 from 2013-15.
Nationally, annual deaths from cardiovascular disease per 100,000 residents increased from an average of 250.8 from 2011-13 to 254.6 from 2013-15, while the average number of cancer deaths per 100,000 residents remained at about 190 a year during both periods.
Arkansas also had the second-highest percentage of adults, behind only West Virginia, who reported frequently being in poor health physically and mentally.
From 2013-16, the percentage of Arkansans who reported that their physical health had not been good for at least 14 of the past 30 days rose from 16.1 to 17.7.
Over the same period, the percentage who reported that their mental health had not been good in 14 of the past 30 days rose from 14.7 to 16.4.
Arkansas did improve in some areas, including in the percentage of children who received recommended vaccinations. In 2016, 67.8 percent of children ages 19 months to 35 months received the vaccinations, up from 66.6 percent in 2015 and 57.1 percent in 2013.
Many of the indicators tracked in the report reflect changes in behavior, Thompson said. For instance, he said, "We used to drink a lot more water, and now we drink a lot more sugar-sweetened beverages."
Other factors, he said, include increased fast-food consumption, neighborhood designs that favor cars over pedestrians and a lack of grocery stores with healthy food in some areas.
The Healthy Active Arkansas plan, endorsed by Hutchinson in 2015, calls on state agencies, businesses, schools and other entities to take steps such as offering nutritious food and implementing workplace wellness programs.
Healthy Active Arkansas, a nonprofit organization formed to implement the plan, on Thursday unveiled a revamped website, healthyactive.org, that offers health tips for individuals, families, employers and other organizations.
Using money from the Delta Dental Foundation, Healthy Active Arkansas in April plans to award $30,000 in grants to schools to install water bottle "filling stations," with the hope that students will drink more water instead of soda.
Thompson said his own office has a "no dumping" policy, barring employees from bringing leftover desserts to put out for their co-workers, and allows employees to take exercise breaks every afternoon.
Marisha DiCarlo, who is leading the state Department of Health's efforts to implement Healthy Active Arkansas, noted that obesity has increased even in healthier states such as Colorado, which had the nation's smallest percentage of obese adults in 2016 and ranked No. 7 in overall health.
"One solution is not going to make a huge impact," DiCarlo said. "We need to look at those things that, put together, can make an impact."
SundayMonday on 12/31/2017