Months of late paychecks and a round of layoffs two weeks before Christmas have stoked fears that a hospital in De Queen will close, former employees and officials said.
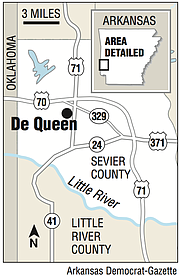
Paychecks expected Dec. 14 weren't distributed until Friday in the most recent sign of distress at De Queen Medical Center, which is the only hospital in Sevier County. On Wednesday, elected officials, business and community leaders, and emergency responders met to discuss contingency plans in case the hospital closes.
"Everybody in town is concerned about it, and there is a lot of talk about it," De Queen Mayor Billy Ray McKelvy said in a phone interview. "Access to health care is a big concern, but of course people have jobs there. ... [If it closed], it'd be terrible."
The hospital's parent company, Missouri-based EmpowerHMS, recently has been late in meeting obligations, including payrolls, rents and utility bills at facilities it owns in Tennessee, Kansas and Oklahoma, according to a range of local-level news reports.
The company's website describes the firm as specializing in helping distressed and underperforming hospitals in rural communities.
Katie Hankins, who had worked three years in the De Queen hospital's housekeeping department, was laid off Dec. 12. She said paychecks for the staff -- including doctors -- have been late since late September or early October. Instead of checks arriving on the Friday payday, they would show up the following Monday, Tuesday or Wednesday, she said.
"They did not let us know ahead of time," she said of company officials. "We just woke up, checked our accounts and the money wasn't there."
Employees stuck it out, Hankins said, because they care about the community and it's tough to find a job so close to the holidays.
A spokesman for the Arkansas Department of Labor confirmed that there is an open wage investigation involving De Queen Medical Center.
Despite troubles meeting payroll, few people were expecting the layoffs, which were not announced in advance and affected about 19 people, Hankins said. She said doesn't know of anyone who was offered severance.
"We literally showed up to work on the 12th, and within five minutes of me arriving, they were calling my name to come up to the office to tell me I was laid off," she said. "That was my home away from home. I think I spent more time there than I did at home with my own family."
Calls to the hospital and EmpowerHMS seeking comment were not returned. A call to the cellphone of EmpowerHMS CEO Jorge Perez wasn't answered, and his voice mail box was full.
Discussion of the De Queen hospital's possible closure has been underway since at least June, when the De Queen Bee ran a lengthy interview with EmpowerHMS hospital network President Michael Christensen.
Christensen had spent two weeks in De Queen meeting with community leaders to dispel rumors of trouble at the medical center, which EmpowerHMS acquired in 2017, according to the newspaper.
In that interview, Christensen touted new services and reorganized leadership at the hospital.
"De Queen Medical Center is not closing its doors," he told the Bee. "We've seen what happens -- communities dry up when the hospital left. People don't want to live where there's no emergency services."
Lisa Taylor, economic development director for Sevier County, said people at Wednesday's meeting discussed plans -- including job placement for workers, and emergency and medical evacuation services -- in case the hospital closes.
"Whether it's now, or a year from now, or 50 years from now, we need to have a plan in place. ... As leaders of the community we need to be prepared," she said.
Officials don't know what specific problems the hospital is facing because the facility is privately owned, she said. As a result, no incentives to keep the hospital in business have been discussed.
Wednesday's meeting, she said, was about basic emergency planning, rather than trying to make payroll for the company.
Rep. DeAnn Vaught, R-Horatio, issued a statement calling the situation "heartbreaking, especially at this time of year. ... The hospital is very important to our area, and we need to support it." She said she's been working with federal and state labor regulators and the Arkansas congressional delegation to address the issue.
Taylor said De Queen Medical Center is among Sevier County's larger employers, though it's not clear how many people work there. It has 22 beds and eight emergency room bays.
A former nurse's aide at the hospital said the hospital is critical to the region because it's one of the few places nearby where health care providers can find work.
"Around there, it's hard to find a good job -- especially as a nurse or [licensed practical nurse], unless you want to drive an hour or 45 minutes," Jennifer Causey said.
Hankins added that the distance to the next-closest hospitals, more than 30 miles away, could amount to life or death for patients.
Michael Murtha, president of the advocacy group National Alliance of Rural Hospitals -- the vast majority of whose charter members appear to be operated by EmpowerHMS, and whose board is headed by Perez -- said it's not unusual for rural medical centers to struggle in December.
At that time, they've often exhausted resources on community and "indigent" care. Such hospitals typically operate on "razor-thin" margins, and administrators often anxiously wait for annual reimbursements to be doled out, he said.
Metro on 12/23/2018