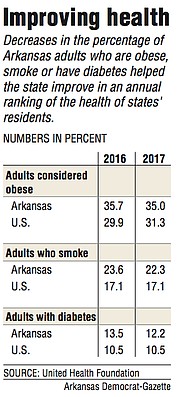
Slight declines in Arkansas' rates of obesity, smoking and diabetes helped the state improve its ranking by two spots, to No. 46, in an annual report on the health of states' residents.
The report by the United Health Foundation, a charity established by Minnetonka, Minn.-based UnitedHealth Group, calculates a health score for each state based on how it compares with the others on more than two dozen measures, using data from a variety of sources.
The latest rankings, released last month, were based largely on data from 2017.
Joe Thompson, chief executive of the Arkansas Center for Health Improvement, said Arkansas' progress is "encouraging" but not yet a cause for celebration.
"When you're at the bottom, there's only one place to go," he said.
"For both the health of our citizens and for the productivity of our state, we need to be in the middle tier of states, and we're not there yet," he said.
Louisiana was labeled the least healthy state, followed by Mississippi, Alabama and Oklahoma.
Hawaii was the healthiest, followed by Massachusetts, Connecticut and Vermont.
Last year, Mississippi ranked last and Louisiana was No. 49.
Thompson said the report highlights Arkansas' high rates of smoking, obesity and physical inactivity, which he called the three biggest contributors to chronic and sometimes fatal health conditions in the state.
In each of those three areas, Arkansas improved slightly or didn't change from 2016 to 2017 while other states got worse, helping Arkansas move up in the rankings.
For instance, in 2016, Arkansas had the country's third-highest percentage of adults who smoke, behind West Virginia, which had the highest rate, and Kentucky, according to U.S. Centers for Disease Control and Prevention survey data used in the report.
The next year, Arkansas' rate fell from 23.6 percent to 22.3 percent, while the rates for Louisiana and Tennessee rose, making Arkansas' rate the fifth-highest.
Similarly, the percentage of Arkansans who are considered obese -- based on their reported height and weight -- fell slightly, from 35.7 percent to 35 percent, while the rates for Oklahoma, Iowa, Alabama and Louisiana rose.
As a result, Arkansas in 2017 had the seventh-highest adult obesity rate in the country. A year earlier, it had tied with Alabama for having the third-highest rate.
In both 2016 and 2017, 32.5 percent of Arkansans reported being physically inactive, meaning they hadn't engaged in exercise outside of regular work duties in the previous 30 days.
That was the highest percentage in the country in 2016.
But the next year, increases in the rates of physical inactivity in Mississippi and Kentucky moved Arkansas to the No. 3 spot for that measure.
A drop in the percentage of Arkansas adults who said they had been diagnosed with diabetes -- a disease that has been linked to smoking, obesity and physical inactivity -- also helped Arkansas' ranking in this year's report.
The state's diabetes rate fell from 13.5 percent in 2016 to 12.2 percent in 2017, moving it from the fourth-highest in the country to the ninth-highest.
Among all U.S. residents, the rates of smoking and diabetes didn't change from 2016 to 2017, while the rates of obesity and physical inactivity rose.
In both years, 17.1 percent of U.S. adults reported that they were smokers and 10.5 percent reported having diabetes.
Meanwhile, the national adult obesity rate rose from 29.9 percent to 31.3 percent, and the physical inactivity rate rose from 23.1 percent to 25.6 percent.
Arkansas health officials have been targeting obesity and physical inactivity through the Healthy Active Arkansas plan, which calls on state agencies, businesses, schools and other entities to take steps such as offering nutritious food and implementing workplace wellness programs.
The state could also enact measures to further reduce its smoking rate, said Gary Wheeler, the state Department of Health's chief medical officer.
Those include raising the minimum age for buying cigarettes, tobacco and vapor products from 18 to 21, increasing the tax on cigarettes from current level of $1.15 a pack and closing gaps in the state's indoor smoking ban.
"There's a whole list of proven policy goals that have not happened in Arkansas," Wheeler said.
Thompson said the state also needs to head off an increase in drug overdose deaths, which partly offset Arkansas' gains in the health rankings report.
Arkansas' overdose deaths increased from an average of 12.3 a year per 100,000 residents from 2013-15 to 13.2 a year per 100,000 residents from 2014-16, according to CDC data cited in the report.
For both time periods, the state's rate was the 14th-lowest in the country.
But CDC data also show that Arkansas had the second-highest rate of opioid prescriptions in 2017, with 105.4 prescriptions per 100 residents. Alabama had the highest rate, 107.2 prescriptions per 100 residents.
As the state and insurers take steps to reduce opioid prescriptions, Arkansas will need more physicians who are licensed to prescribe drugs that treat opioid addiction, Thompson said.
"We have not yet had as much of an influx of illicit drugs," such as heroin, Thompson said. "As restrictions are placed on prescribers, if we don't have physicians treating people who are addicted, [the patients] will turn to those illicit drugs, and we will start to see those death rates go up."
The report docked Arkansas points for a decrease in the percentage of boys age 13-17 who had received the recommended doses of the human papillomavirus, or HPV, vaccine -- the only vaccine tracked in the report that isn't required for children in Arkansas schools.
From 2016-17, the percentage of girls in that age range who had received the recommended doses increased from 35.5 percent to 46.6 percent, but the percentage for boys dropped from 33.6 percent to 24.3 percent.
Because of the changes in rates, the state's ranking for the percentage of girls who had received the vaccine climbed from No. 47 to No. 39 while the rate for boys fell from No. 35 to No. 49, ahead of only Mississippi.
By contrast, more than 90 percent of Arkansas children age 13-17 had received two other vaccines, for meningococcal disease and the so-called Tdap vaccine for tetanus, diphtheria, and pertussis in 2017.
Both vaccines are required for children attending public or private schools.
Wheeler said a stigma associated with HPV has prevented some parents from getting their children immunized against the sexually transmitted virus. That has been changing, he said, as public health officials have emphasized the vaccine's importance in preventing cancers caused by HPV.
"It's one of the most easily achievable successes that we can have in modern medicine," Wheeler said. "All you have to do is make sure that every kid has the vaccine, and we're going to see a dramatic drop in the amount of cervical cancer and oral cancer that adults get later in life."
A Section on 01/02/2019