Nineteen Arkansas nursing homes will be among the nation’s first to receive quick-response coronavirus test machines under a federal program announced in July.
T h e a n n o u n c e m e n t comes as some experts express reservations about the devices and the accuracy of testing they provide, which one virologist called “a potential source of false security.”
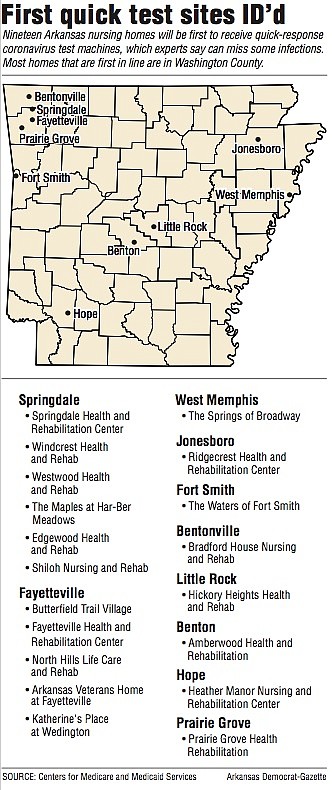
The scheduled recipients are scattered statewide: Springdale to Hope to West Memphis, including nursing homes in Fayetteville, Bentonville, Prairie Grove, Little Rock, Benton, Jonesboro and Fort Smith.
The facilities appear on a list of 2,425 nationwide prioritized to receive the first round of machines supplied by the U.S. Department of Health and Human Services.
More than 3,900 nursing homes eventually should get the devices that calculate positive or negative results within about 15 minutes, federal officials said. The U.S. has roughly 15,500 nursing homes.
Because the machines test for covid-19 antigens, they are “definitely not the best-case scenario for these types of vulnerable populations,” cautions Joseph Petrosino, chairman of molecular virology and microbiology at Baylor College of Medicine. Antigen testing is “prone” to false negative results for infected people who have no symptoms, he said.
“The biggest threat to a nursing home isn’t necessarily the person who’s already sick,” the scientist continued. “It’s the asymptomatic carrier, and these tests are not really well-developed for that type of surveillance purpose.”
Potential false negatives mean tests run the risk of being “useless,” said Martha Deaver, president of Arkansas Advocates for Nursing Home Residents. If tests might show negative results for people infected with covid-19, “how can the employees safely be around” nursing home residents, she asked.
A Washington, D.C.-based aging services advocacy network sent a letter to federal testing czar Adm. Brett Giroir on Wednesday, citing reports of a 20% false negative rate for antigen testing machines.
The Arkansas Department of Health, and the federal Health and Human Services Department recommend further testing to verify that someone who tests negative in an antigen test is not actually infected with the virus.
“The need for retesting will lead to the same concerns our members have been experiencing: limited supply of tests and increasing turnaround times for results,” LeadingAge President Katie Smith Sloan wrote.
Experts say the gold standard to detect the novel coronavirus is a polymerase chain reaction, or PCR test: a sensitive, laboratory-processed test that looks for the virus’s genetic material. Those tests don’t detect infections perfectly, but are the most accurate available, scientists agree.
Antigen tests — not to be confused with antibody tests, which identify previous infections — work differently, identifying active infections via proteins. In the widely circulated illustration of the virus, that’s a part of the spike that sticks out of the ball, Petrosino said.
The Food and Drug Administration approved two antigen tests for the virus under emergency-use rules in May and July. One of those tests’ negative results “do not rule out [covid-19 infection] and should not be used as the sole basis for treatment or patient management decisions, including infection control decisions,” an approval letter says.
Such qualifiers raised questions, including in a list of “frequently asked questions” about the federal program to send antigen tests to nursing homes. One asked why antigen tests are heading to centers with more elderly and ill populations, where results are high stakes.
“Fighting this global pandemic requires an array of different technologies, including antigen testing,” a response reads in part.
Arkansas Health Care Association executive director Rachel Bunch said in an interview that “there’s still a lot of unknowns” about the forthcoming test devices. The group, which represents nursing homes in the state, will work with the Health Department to learn how best to make use of the machines, she said.
An Arkansas Department of Health spokeswoman framed accuracy concerns as a “small chance” of false negative results. At a news conference on July 24, interim Health Secretary Dr. Jose Romero lauded the testing-machine program, saying it will help identify infections in nursing homes quickly.
“I think we’re going to have better control of this in the next few months as we begin to have these point-of-care tests placed in these institutions,” he said.
Rajendram Rajnarayanan, assistant dean of research at New York Institute of Technology College of Osteopathic Medicine at Arkansas State University, agreed that antigen-testing machines aren’t as accurate when they give negative results, but said a positive result from that test is reliable, and he supports the initiative for that reason.
No test is perfect, he said. That’s important to remember when processing delays and supply shortages hinder use of other types of tests. For nursing homes, “something is better than nothing right now,” he said.
Federal materials say nursing homes were prioritized to receive testing machines based on factors that include geographic hot spots, new resident cases or new deaths from covid-19.
Shipments are expected within four weeks but may take “as long as 14 weeks … due to supply availability,” a fact sheet said.
Administrators for three of the Arkansas nursing homes — Butterfield Trail Village in Fayetteville, and Edgewood Health and Rehab and Westwood Health and Rehab, both in Springdale — said they had not yet received the machines or notice of delivery dates. Several others did not return messages seeking comment last week.
DESPITE NEGATIVES
Like others across the U.S., Arkansas’ nursing homes have battled covid-19 outbreaks. As of Friday, the Health Department had logged infections in residents or staff members at 153 of the state’s 226 nursing homes. At least 147 residents have died.
[CORONAVIRUS: Click here for our complete coverage » arkansasonline.com/coronavirus]
Infections spread quickly in such settings because of close quarters, and contacts among residents and caregivers. Inspectors also noted infection-control failures, such as lapses in hand-washing, at some Arkansas facilities, the Arkansas Democrat-Gazette reported in May.
The antigen testing-machines program is part of expanded federal efforts to beat back the virus. Regulators will soon require nursing homes to test all staff members weekly in states where 5% of test results have come back positive, which includes Arkansas.
Bunch says her group is “optimistic” about the prospect of the rapid testing machines, but agreed that the prospect of unreliable results was worrisome. It also may become difficult for nursing homes nationwide to buy test kits for the machines, which is not something facilities have done before, she said.
At commercial rates, testing kits for the antigen machines cost $20-$25 per unit, said a spokeswoman for the Centers for Medicare and Medicaid Services, which oversees nursing homes. She declined to say how much the federal agency paid for testing kits because “we don’t share contracting cost information.”
Kelly Hale Syer, marketing director for Butterfield Trail Village in Fayetteville, said there are concerns about procuring supplies and what would happen if someone who is infected tests negative, “potentially putting others at risk.” But administrators there “believe an antigen test program is far superior than no testing at all,” she wrote in a prepared statement.
Ed Holman, owner of Indian Rock Village Health Center in Fairfield Bay, said he’s “excited about the potential” for lower-cost, rapid-result testing “even with the [possible false] negatives.”
“I’m kind of going on the odds if we test staff every 3 to 4 days, I’m kind of hoping if [someone is] positive, it will show up in 1 to 2 tests,” he said.
Testing at that frequency will require money, as nursing homes will shoulder the costs for testing kits. While some of those costs may be calculated into future reimbursement rates, “some state money would certainly help with the testing” in the interim, Holman said.
“That would encourage everybody to [test frequently]. They wouldn’t have an excuse not to,” he said, adding that nursing homes statewide are collecting less money as admissions decline.
‘IMPORTANT INFORMATION’
One quirk of the federal program is that its allocation criteria meant several Arkansas nursing homes with serious outbreaks aren’t first in line. Of the 19 homes to first receive testing machines, 10 haven’t recorded a single covid-19 case among residents since the pandemic began, according to Health Department data Friday.
Deaver, the nursing home residents’ advocate, said it was “very concerning” that homes such as Mitchell’s Nursing Home in Danville, which had 74 resident infections, weren’t included in the first round.
A Department of Human Services official said there were no plans to redistribute testing machines to harder-hit homes. The agency hasn’t heard much about the program from federal counterparts, said Jerry Sharum, the state’s Division of Provider Services and Quality Assurance director.
Testing machines will be sent directly from manufacturers to nursing homes, and the state’s Office of Long-Term Care won’t be involved, he said.
State Health Department spokeswoman Danyelle Mc-Neill referred most questions about that agency’s involvement with quick-test machines sent to nursing homes to the Arkansas Health Care Association, the nursing-home lobbying and advocacy group.
Gov. Asa Hutchinson recently announced at a news conference that Arkansas has purchased 200 antigen quick-test machines to aid its virus response. The state will track the results separately from a lab-confirmed case count, he said at a briefing last week.
The state’s machines should arrive in mid-August “or possibly sooner,” McNeill said. Officials still are debating how to deploy them.
Researchers work constantly on new testing methods, said virologist Petrosino, trying to get around supply-chain clogs and other issues that stifled the national ability to conduct and process tests. For the most accurate PCR tests, the issues look unlikely to change in the immediate future, he said.
“It’s probably going to take a nationwide tamping down of the virus, or reduction of prevalence of the virus, to get the manufacturers to catch up,” he said.
Information for this article was contributed by Eric Besson of the Arkansas Democrat-Gazette.