Arkansans in a state of psychiatric crisis may find themselves waiting up to a month to secure a bed in an inpatient psychiatric facility.
This is due to the increase in those seeking help with symptoms of anxiety and depression amid the covid-19 pandemic.
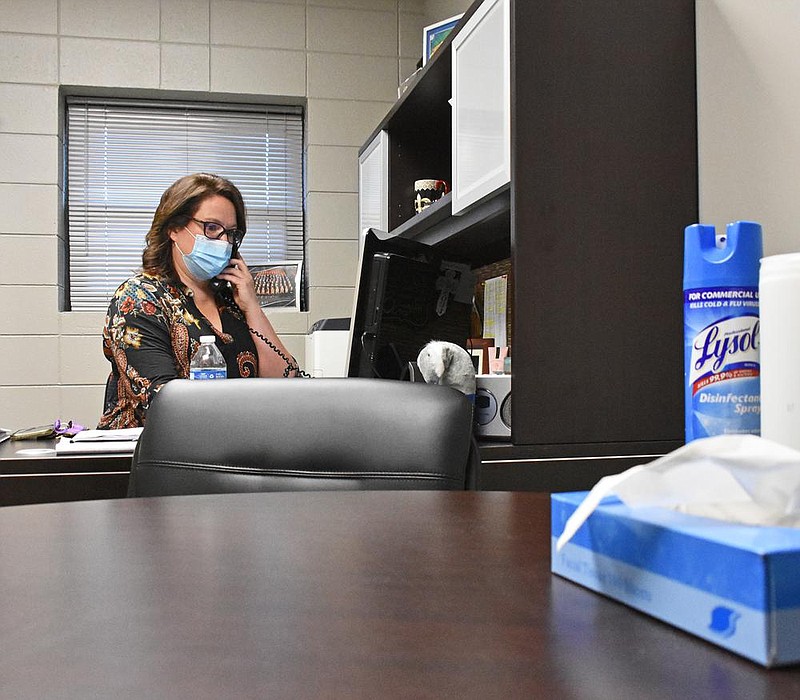
“There’s most definitely a wait list,” said Peggy Kelly, chief clinical director at Youth Home, a private nonprofit mental health provider that offers both inpatient and outpatient services for youth. The top diagnoses Youth Home treats in its residential program are depression, anxiety and trauma, according to Kelly.
In late June of this year, the Centers for Disease Control and Prevention conducted a survey on adverse mental health outcomes, increased substance use and suicide ideation during the pandemic.
Almost 75% of the 731 respondents between the ages of 18 and 24 reported experiencing an adverse mental or behavioral symptom.
Of that same group, about a fourth of that age group had considered suicide in the past 30 days. Additionally, a fourth of that group started or increased substance use to cope with pandemic-related stress.
According to Kelly, kids who experienced trauma in early childhood and are now living through the pandemic find it difficult to cope.
“Navigating any kind of change in their environment is more challenging,” the director said.
TIPS TO EASE SYMPTOMS:
Try to focus on the things you can control right now, recommends Greg Adams, a social worker at Arkansas Children’s Hospital. Some recommendations he gives include:
• We can connect with people, though it looks different from what we’re used to.
• We can choose to seek out accurate information and control how much information we want to take in to avoid information overload.
• We can change our perspective by seeing the holiday season as an opportunity where we have more time and less demand, which may offer us a quieter more reflective holiday experience.
• Parents can try to create as much reasonable structure in their kids’ lives as possible Adams said. They can set expectations about when their kids do school and when they have breaks, he added. “They do better when things are predictable,” he said. Parents can still get some of their kids’ other needs met, like interacting outdoors with smaller groups or virtually, despite the pandemic’s limitations.
Prior to the pandemic, Kelly said patients were admitted about a week after paperwork was completed and insurance was verified. Now wait times are at least two months for the inpatient program, she said.
There is some good news, though. “There is a lot of help available on an outpatient basis right now. We’re normally able to get people an appointment pretty quickly,” she said.
The Arkansas chapter of the National Alliance on Mental Illness is noticing similar problems with admission wait times.
“It’s horrible actually. Since covid’s come, a lot of hospitals, they’re not even taking patients unless they go to the ER and have testing,” said Buster Lackey, executive director of NAMI-Arkansas.
As a result of the pandemic, many hospitals have restricted their beds to the most serious cases, Lackey said, though the admission policy during covid will likely be different at every hospital.
If the individual is considered suicidal or homicidal, the staff gets them inpatient care, but it’s takes longer because they have to jump through hoops to make sure they’re covid-free and not experiencing symptoms, Lackey added.
If the individual is not suicidal or homicidal, Lackey said they likely won’t get inpatient care, but will instead be referred back to their therapist for outpatient care.
“Many [hospitals] are requiring people seeking to be admitted to go to the local ER to be medically cleared. This causes undue stress on the ER staff and more stress for the person seeking mental health help,” Lackey said. “I would think that many just will not go to the ER and therefore will not get the help they need.”
HOW TO START A CONVERSATION ABOUT MENTAL HEALTH:
Peggy Kelly, chief clinical director at Youth Home, recommends remembering the “three Cs” when starting a conversation about mental health: care, concern and consequences.
• Care: Approach the person with a genuine statement about how much you care for them.
• Concern: Note behaviors you have seen that are out of character from them, taking care not to give more than three.
• Consequences: Help them look down the road at what might be the natural consequences of their behavior.
• Finally, end with “I would really like to help you reach out and get some professional help,” she said.
You don’t have to know what to say, says Buster Lackey, executive director of NAMI-Arkansas. It can be as simple as sitting down, starting off with your story and easing into a conversation.
“Be direct, honest, and caring. Listen fast, speak slowly,” he says.
Adams recommends saying “I’m feeling this way, what’s it like for you?” or “I’m having a bad day, how about you?” People will respond better if someone’s willing to disclose how it is for them, he says.
Lackey said some hospitals are offering partial hospitalizations, in which a person goes to a clinic for half a day, or sometimes the whole day, then returns home at night.
Isolation is the primary thing Lackey said people are struggling with. He related this to people’s fight-or-flight responses. In normal times kids can go to school, parents can go to work, letting them get away from a particular situation, regroup and come back. Now, all people can do is “fight," he added, with every minor thing that happens capable of “setting a person off.”
“I wish they would not have called it “social distance," but “physical distancing," Lackey said, adding that the term can lead some people to believe they cannot leave their house at all.
He recommended people get out for walks and get exercise to open their lungs.
Lackey, who also runs a private social work practice in North Little Rock, recommends that, even if multiple places have said they don’t have space, patients shouldn’t lose hope.
“Any community mental health center, there will be a therapist that will see you,” he said. “Many private practices will, even for an abbreviated session.”
At Youth Home, because they're trying to keep the kids in residential care safe from covid, kids aren't getting passes to go home for the weekend, Kelly said.
"Family connection is really important, because we're working on healing the whole family," she said.
While kids have been in residential care amid the pandemic, they have had grandparents who have passed away, parents with medical conditions, and the kids want to go home to be with them and they can't, Kelly added.
"I worry somewhat about family connection and how that's going to be affected for these kids," she said.
In lieu of those in-person visits, the treatment center has been relying on Zoom calls as often as they can, Kelly said.
RESOURCES AVAILABLE:
• National Suicide Prevention Hotline: (800) 273-8255, text 741741 or visit https://suicideprev…">suicidepreventionli… for 24/7 support.
• NAMI Arkansas: Coordinates a network of local support groups providing support, education and advocacy. NAMI has support groups in Little Rock, Cabot, Conway, Texarkana, Fort Smith, and Springdale. For dates and times, visit https://namiarkansa…">namiarkansas.org or call (800) 844-0381 or (501) 661-1548.
• Substance Abuse and Mental Health Services Disaster Distress Helpline: (800) 985-5990, 24/7 365-days-a-year crisis counseling and support to people experiencing emotional distress related to natural or human caused disasters.
• Good Mourning Program at Arkansas Children’s Hospital: An eight-week support group held in the spring and fall for children who have lost someone important in their life; adults connected to children participate can participate as well. Visit https://www.archild…">archildrens.org/cen….
• Arkansas Children’s Hospital: there are two behavioral health resource coordinators that work to help families find available resources in their community. They are meant to help problem-solve and work to match families based on need with what’s available, said social worker Greg Adams. They can be contacted at (501) 364-4411.
• Online support groups: https://www.7cups.c…">www.7cups.com offers free 24/7 chat and affordable online therapy; www.emotionsanonymo… is an anonymous program that offers both free online remote meetings and face-to-face support groups, available in different languages.
• Apps on your smartphone: These include meditation apps Headspace (free trial, and then $13/month) and Calm (free trial, and then $6/month).