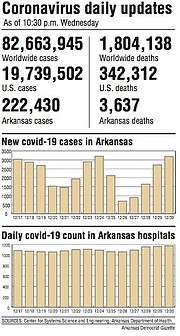
Arkansas' count of coronavirus cases rose Wednesday by 3,184 -- the second-highest one-day jump since the start of the pandemic.
The number of covid-19 patients in the state's hospitals rose by 13, to 1,174, setting a new high for the third day in a row.
Those patients included 205 who were on ventilators, up from 198 a day earlier.
The state's death toll from the virus, as tracked by the Department of Health, rose by 34, to 3,637.
"We continue to see high numbers of new cases and capacity pressures on our hospitals," Gov. Asa Hutchinson said in a statement.
"I urge everyone to be careful as we enter another holiday to reduce the virus spread, and we need to support each other as Arkansans while we work to distribute the vaccine."
[CORONAVIRUS: Click here for our complete coverage » arkansasonline.com/coronavirus]
Wednesday's increase in cases was just the third one-day jump since the start of the pandemic that has topped 3,000 and the largest one that has happened on a Wednesday.
The biggest increase was the 3,204 cases added to the state's count on Dec. 24.
The number of patients on ventilators set a record for that metric as it's reported in the Health Department's daily updates, but was below the high of 211 patients that the department reported on its online dashboard as of Nov. 30.
"I am really concerned that we have not seen the surge from Christmas yet, and already we have a record number of people on the ventilator," state Epidemiologist Jennifer Dillaha said.
Although the state this week entered its third week of administering coronavirus vaccines, focusing initially on health care workers and long-term-care residents and workers, Dillaha said it will be "several months" before enough Arkansans have been immunized to begin having an impact on cases and hospitalizations.
"It is hard for me to imagine how much worse it's going to get," she said.
"I think it's entirely likely that it will get worse, but this is new territory, and I would not at this time hazard a prediction about how much worse."
[Interactive Arkansas map not showing up above? Click here to see it: arkansasonline.com/arvirus]
PRISONS ON 'LOCKDOWN'
An increase in cases among staff members prompted the Department of Corrections on Wednesday to announce a "lockdown" of the state's prisons until at least Jan. 15.
As of Tuesday, 192 of the department's employees were on leave after testing positive for the virus, the department said in a news release.
The lockdown status means that "all non-essential movement within facilities or between facilities will be suspended," and a visitation pilot project launched earlier this month at four state prisons will be suspended, the department said.
Only "emergency intakes" of inmates from county jails will be scheduled, it said.
"The goal of this lockdown is to lessen the impact of the increase in community cases," Secretary of Corrections Solomon Graves said in the release.
The department said Graves urged staff members to take precautions, such as wearing masks, washing their hands and practicing social distancing.
VACCINE PLANS
Also Wednesday, Dillaha said the state's focus next week for the vaccine developed by Pfizer and BioNTech will move from workers in the state's hospitals to those who work in clinics and other settings.
Those eligible for the shots will include staff members at primary care and urgent care clinics, dental clinics, pharmacies, blood donation centers, dialysis centers and university health clinics, as well as school nurses, home health and private care aides, and hospice workers.
Shots will also be available for ambulance workers who have yet to receive them, Dillaha said.
"We have been able to provide vaccines to hospitals to cover their high-priority workers, and so now we're shifting our attention to high-priority health care workers that don't work in hospitals or long-term-care facilities," Dillaha said.
She said the vaccine will be shipped to pharmacies that have agreed to help vaccinate health care workers.
"The pharmacies will be reaching out to the various clinics and entities in their communities to arrange for vaccinations," Dillaha said.
"They'll be asking them to identify their high-risk workers."
[Interactive tables not showing up above? Click here to see them: arkansasonline.com/schools]
She said the "high-risk workers" include those involved in patient care. Administrative staff members and others who aren't involved in patient care will be covered in a future round of vaccinations.
About 140 pharmacies around the state have agreed to participate in the effort, Dillaha said.
She said she didn't know yet whether they will all receive the vaccine next week but she hoped to provide it to "as many as possible."
So far, the state's allocation of the Pfizer vaccine has been directed primarily to high-priority workers in hospitals, including general acute-care, psychiatric, rehabilitation, long-term acute-care and surgical hospitals.
The Corrections Department also received doses for workers at prison infirmaries and the hospital in the Ouachita River Unit in Malvern.
Hospitals have also been able to vaccinate high-priority workers at affiliated clinics and also ambulance workers.
Dillaha said two drugstores in Saline County -- Bryant Family Pharmacy and West Side Pharmacy in Benton -- each received 975 doses of the vaccine this week as a "practice run" at providing the vaccine to the types of workers who will begin receiving the shots next week in larger numbers.
"They had worked together to plan how they would do this, so we provided vaccine to those two pharmacies to do vaccinations for community-based health care workers," she said.
Another pharmacy received doses this week to be administered to workers at Little Rock-based CARTI, which operates several cancer treatment centers around the state.
Through the end of this week, the state has been allocated a total of 92,625 doses of the Pfizer vaccine and 68,800 doses of the Moderna vaccine, the latter of which the state initially designated for residents and workers in nursing homes and other long-term-care facilities.
The state on Wednesday received the last of this week's allocation of 48,750 doses of the Pfizer vaccine, including 25,350 doses that will be used next week to provide booster shots for those who received their first shots earlier this month.
The total allocation so far of the Moderna vaccine, which began arriving last week, has included 37,100 doses that went to Walgreens and CVS as part of a federal program to vaccinate residents and workers at long-term-care facilities.
An additional 31,700 doses went to other pharmacies in the state that will provide the shots at other long-term-care facilities.
Health Department spokesman Gavin Lesnick said the department didn't yet know how many doses of the vaccines the state will get next week.
SHOTS CONTINUE
As of Wednesday morning, providers reported administering 22,673 of the 65,235 doses of the Pfizer vaccine that had been received at that time and 3,006 of the 31,700 doses of Moderna vaccine that went to pharmacies other than CVS and Walgreens.
The two national pharmacies reported administering 84 doses, Health Department spokeswoman Danyelle McNeill said.
Pharmacies and other providers have three days to report the vaccines they administer, so the actual number of shots given is higher than the Health Department's figures.
Little Rock-based Baptist Health's hospitals had administered a total of nearly 6,000 doses as of late Wednesday, spokeswoman Margot Vogel said.
The hospitals will continue vaccination efforts through today, then take a break through the holiday weekend.
CHI St. Vincent Infirmary-Little Rock spokeswoman Bonnie Ward said the hospital had given more than 2,400 shots so far.
"Vaccinations will continue among our staff in anticipation of more doses of the vaccine delivered each week," Ward said. "Due to the nature of the vaccine, each of those vaccinated will require a second vaccination within 21 days. Our ministry anticipates the first shipment of the second doses of the vaccine next week."
David Fortner, vice president of operations for Mercy Hospital Northwest Arkansas in Rogers, said the hospital had administered about 1,500 doses of the vaccine as of the end of the day Wednesday.
"Mercy received a shipment Wednesday, as promised by Pfizer, to provide a second dose to front-line co-workers beginning Tuesday, Jan. 5," said Fortner, who is also a licensed pharmacist. "At the same time, we continue to vaccinate co-workers by priority with their first dose."
UAMS Medical Center is out of the vaccine after administered more than 3,400 doses since Dec. 14, spokeswoman Andrea Peel said.
"As soon as shipment arrives we will prepare for administering the next round of first-time vaccinations and second shot for those who received their first dose earlier," Peel said.
St. Bernards Medical Center spokesman Mitchell Nail said the Jonesboro hospital has administered 2,789 vaccine doses so far.
"This week's vaccinations will end New Year's Eve," Nail said. "We're still vaccinating staff members who were unavailable the week before and of Christmas, as well as first responders, public servants and partner providers."
FEW DECLINE
Ward said the CHI St. Vincent staff has had a "very positive" response to the vaccine offering.
"Only a very low number of staff have declined to receive the vaccine. A limited number of staff have also chosen to wait to see how the process goes and are now opting to receive the vaccine," Ward said. "CHI St. Vincent encourages vaccination against covid-19 among our staff, but it is not required."
Peel said only "very few" staff members have decided against taking the vaccine.
Fortner said there is no process for employees to decline the vaccine because it is not mandated.
"Anecdotally, we know that some co-workers don't plan to get the vaccine at this time, for a variety of reasons," he said.
Likewise, Nail said St. Bernards employees are under no obligation to get the shots, and there will be no adverse action taken against those health care workers who choose not to participate.
"We have safeguards in place at St. Bernards Medical Center that protect unvaccinated patients and their support persons should one of our team members refuse the vaccine," Nail said. "These protective measures include universal screenings and masking, as well as social distancing and good hygiene requirements."
When asked if there were any repercussions for health care workers who choose not to be vaccinated, Peel said UAMS has "not had to make any adjustments to anyone's work duties yet." When asked for further clarification, Peel said an employee will not be terminated for refusing the vaccine because "it's not mandatory."
"All I can tell you is, right now, we are not reassigning people," Peel said.
Regardless, if some staff members decline the vaccine, all doses will be used, Ward said.
"The goal of the vaccination effort at CHI St. Vincent is to utilize all six doses included in each vial, and we have not encountered any issues preventing full utilization at this time," she said.
Nail said St. Bernards' scheduling and logistics teams "have done remarkable work" to ensure employees arrive on time and the proper number of doses are ready and available. Should someone not show up, a substitute would be found to take that dose.
"We consider each vaccine an incredible resource and a great responsibility, too," Nail said. "To steward that resource, we will not let doses go to waste."
Fortner said Mercy Hospital has created a clinic-type vaccine setting where co-workers can come in on their timetables to get the vaccine.
"We have been fortunate not to have to dispose of any vaccine for any reason," Fortner said.
Peel said UAMS has used every dose given to the academic medical center.
"We have employees waiting throughout the campus," she said.
THE NUMBERS
The cases added Wednesday to the state's tallies included 2,320 that were confirmed through polymerase chain reaction, or PCR, tests.
The other 864 were "probable" cases, which include those identified through less-sensitive antigen tests.
The state's cumulative count of cases rose to 222,430.
That comprised 184,947 confirmed cases and 37,483 probable ones.
The number of cases that were considered active rose by 672, to 21,853, as 2,478 Arkansans were newly classified as having recovered.
The state death toll from the virus rose by 26, to 3,068, among confirmed cases and by eight, to 569, among probable cases.
Among nursing home and assisted living facility residents, the state's count of virus deaths grew by 16, to 1,503.
The number of people who have ever been hospitalized in the state with covid-19 grew by 103, to 11,271.
The number of coronavirus patients who have ever been on ventilator because of covid-19 rose by 13, to 1,212.
Pulaski County had the largest number of new cases, 355, followed by Washington County with 290, Benton County with 278, Faulkner County with 150 and Sebastian County with 134.
Among prison and jail inmates, the Health Department's count of cases rose by 31.
Corrections Department spokeswoman Cindy Murphy said the number of cases among inmates rose by 15 at the Central Arkansas Community Corrections Center in Little Rock, by eight at the Barbara Ester Unit in Pine Bluff, by six at the Wrightsville Unit and by two at the Omega Supervision Sanction Center in Malvern.
The Tucker Unit in Jefferson County and Varner Unit in Lincoln County also each had one new inmate case.
Among those prisons, the Ester Unit had the largest number of cases that were active, 144, followed by the Tucker Unit, which had 62, and the Little Rock lockup, which had 38.
UAMS ADJUSTS
UAMS Chancellor Cam Patterson said in a series of tweets Wednesday that the university's hospital "has had difficulty keeping pace with the needs of patients with & without COVID-19."
"Our next steps here at UAMS include asking our healthcare providers to take on more patients than usual, to reassign some of them to new duties that they are capable of, & potentially to start doubling up patients in single rooms," Patterson said.
He said the hospital is also constructing an addition to is emergency department in the adjacent parking deck for "triage and other purposes."
"Hopefully nothing more is needed, but if it is, we have more arrows in our quiver," he said. "You can help us by thanking those who work in health care for the work that they are doing under these difficult circumstances, & more importantly abiding by the principles of masking & social distancing."
Peel said UAMS has created a new covid-extender registered nurse position, for nurses who don't normally work in patient care, to help meet the staffing demands.
"We also introduced a team-based care model which allows non-ICU nursing staff to provide patient support for intensive care patients and covid-extenders to help care for other patients," Peel said. "This model will allow nursing staff to care for more patients than their typical ratio while ensuring our quality and safety standards are maintained."
UAMS is using new surgical techniques to help reduce overnight stays for elective surgeries and are rescheduling some elective surgeries and procedures until a later date, she said.
The hospital is at ICU max -- all 64 critical care beds in use -- "with a few set aside" for in-house patients who may need to be upgraded, Peel said.
At St. Bernards, Nail said the census numbers "have been high lately as we near January and February; typically our busiest months of the year."
"As such, we find ourselves making those changes more often than not based upon our heavy patient loads," Nail said. "We have open beds, but our available space is limited."
The Jonesboro hospital has no plans to delay any regular services or elective surgeries, which it considers "vital to our community's overall health," Nail said.
Ward said CHI St. Vincent Infirmary-Little Rock "continues to experience a high level of capacity at our hospitals from a wide range of patients in need of critical care at this time of year, as well as patients with covid-19 who require hospitalization."
"Our hospitals remain prepared to provide quality, compassionate care to all those in need and would encourage members of the community not to delay their critical care needs," Ward said.
The hospital also continues to schedule elective procedures.
"CHI St. Vincent also encourages those in the community not to delay their critical care needs," Ward said. "Virtual visits, more stringent sanitization processes, universal masking and other new processes are in place to help ensure they can continue to receive preventative and ongoing care safely without allowing their condition to worsen to the point that it requires a visit to the emergency department."
Each St. Vincent facility has a surge capacity plan that is "continuously reviewed to ensure" the hospital is prepared to effectively care for all patients, she said.
"We are very thankful for our health care workers as they remain focused on caring for patients with varying needs and illnesses at this challenging time," Ward said. "Our challenge is to ensure that we are caring for our health care heroes. We have spent time making action plans based on a recent Engagement Survey to identify their needs and have established clear lines of communication. We are also working diligently to provide resources that address wellness, stress and other issues they face."
ICU BEDS SCARCE
The number of available critical care beds in the state dropped by five to 50 Wednesday -- the lowest point in nearly two weeks.
Out of the state's 1,155 inventory of ICU beds, 96% are in use.
The number of hospital beds available for use increased by 44, going from 1,924 to 1,968 Wednesday.
The total beds -- whether filled or vacant -- dropped by 16 from 8,940 to 8,924. The total includes more than 300 in psychiatric or rehabilitation facilities that aren't for covid-19 care.
That means about 78% of the state's hospital beds are full.
The state inventory of ventilators remained the same at 1,091.
About 59.5%, or 650, ventilators remain available for use, one more than the day before.
Total bed capacity -- hospital beds that can be staffed whether or not they are occupied -- dropped by 16 beds to 8,894.
The 16-bed loss was attributed to hospitals in the northwest region of the state, according to Health Department data.
Maximum flex bed capacity -- the number of hospital beds regardless of ability to staff them -- dropped by 56 beds to 11,428.
The 56 beds were lost from hospitals in the southwest region of the state, according to the Health Department.
The majority of the 1,174 covid-19 patients hospitalized -- 368 -- were in hospitals in the metropolitan region of the state followed by 201 in the southwest, 150 in the northeast, 141 in the Arkansas Valley, 129 in the northwest, 119 in the north-central and 66 in the southeast.
Metro region hospitals also had 158 patients in ICU followed by 65 in the southwest, 55 in the northwest, 37 in the Arkansas Valley, 29 in the northeast, 26 in the north-central and 15 in the southeast.
The hospitals with the highest number of patients on ventilators were in the metro region with 90, followed by the southwest with 32, northwest with 23, Arkansas Valley with 20, northeast with 18, north-central with 18 and southeast with four.