Federal officials have asked for expedited consideration of their appeals of rulings that struck down Medicaid work requirements in Arkansas and Kentucky.
In a filing Thursday with U.S. Court of Appeals for the District of Columbia Circuit, officials said the rulings by U.S. District Judge James Boasberg of Washington, D.C., disrupted demonstration projects in the two states and created uncertainty about whether work requirements that have been approved in other states will also be thrown out.
Boasberg's "orders have caused and will continue to cause significant disruption to the detriment of States and the federal government, which looks to the results of demonstration projects to determine fruitful courses of action in administering the Medicaid program," U.S. Department of Justice attorneys representing the Department of Health and Human Services Department wrote in the filing.
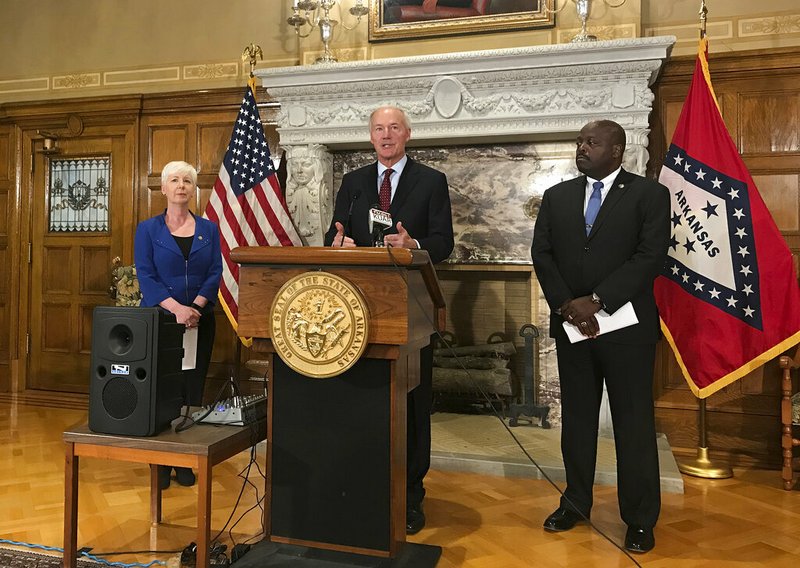
Gov. Asa Hutchinson said in a statement Friday that he was "delighted that the Department of Justice followed through with the request for an expedited appeal, as I expected they would."
"The timeline that they have outlined to the D.C. Court of Appeals is a very fast and workable schedule that will allow the D.C. Court of Appeals and, if necessary, the U.S. Supreme Court to hear this case in a timely fashion," he said.
According to the appeals court's procedures handbook, such requests for expedited consideration are granted "very rarely" and only when a delay would "cause irreparable injury" or when "the public generally, or in which persons not before the Court, have an unusual interest in prompt disposition. The reasons must be strongly compelling."
Sara Rosenbaum, a health law and policy professor at George Washington University in Washington, D.C., said the dispute over work requirements isn't the type of case that would usually merit such consideration.
She was one of dozens of health policy professors and researchers who submitted briefs in support of the plaintiffs in the two cases.
"There's nothing urgent about this at all," she said, adding that Medicaid expansion in Arkansas is "working quite well" without the requirement.
"What you have is an angry administration that wants to be allowed to do something that the courts are saying they can't do," she said.
Kevin De Liban, an attorney for Legal Aid of Arkansas, said the plaintiffs will file a brief opposing the request for expedited consideration. That response is due Tuesday, according to a scheduling order issued by the appeals court Friday.
The Jonesboro-based group is one of three organizations that filed the suit challenging Arkansas' requirement on behalf of several enrollees.
Under the expedited schedule proposed by the Health and Human Services Department, the final briefs in the appeals would be due July 30, and oral arguments would be held "during the first week after the summer recess."
The department asked for a decision to then be issued "at the earliest possible time so that the projects can go forward and so that, after this Court's decision, the losing party would be afforded an opportunity to decide whether to ask the [U.S.] Supreme Court to consider the cases before the end of the next term."
According to the Supreme Court's website, terms end in June or July. That would make the end of the next term in June or July of 2020.
Boasberg on March 27 found that Health and Human Services Department, in approving work requirements in the two states, violated the law governing Medicaid by failing to consider the effect such requirements would have on the program's goal of providing health coverage to needy people.
Arkansas' requirement, which took effect in June, resulted in 18,164 enrollees losing coverage. Boasberg's ruling preserved coverage for an additional 5,492 enrollees who did not meet the work requirement for January and February and had not yet met it for March when the ruling was issued.
To stay in compliance, enrollees had to spend 80 hours a month on work or other approved activities, unless they qualified for an exemption, and report what they did using a state website or over the phone.
Those who failed to meet the requirement for three months during a year were kicked off the program and barred from re-enrolling for the rest of the year.
The requirement, the first ever implemented for Medicaid enrollees in the more than 50-year history of the program, applied to enrollees of Arkansas Works, as the expanded part of the state's Medicaid program is known.
The expansion in 2014 extended coverage to adults with incomes of up to 138 percent of the poverty level. This year, for instance the income cutoff is $17,236 for an individual or $35,535 for a family of four.
Federal officials have argued that such requirements promote the fiscal sustainability of Medicaid by prodding enrollees to find jobs and move off the program. They also argue that people who work tend to be healthier than those who are unemployed.
Boasberg said in his ruling that the Health and Human Services Department didn't weigh those potential benefits against the harm that kicking people off of Medicaid for noncompliance would cause to their health and the program's goal of providing health coverage.
In the filing Thursday, the Health and Human Services Department contended that Boasberg's rulings resulted from "a basic misunderstanding of the nature of a demonstration project."
Section 1115 of the Social Security Act allows such projects that the Health and Human Services Department secretary determines are "likely to assist in promoting the objectives" of Medicaid.
"The point of these experiments is to test hypotheses, and either validate a hypothesis that might lead to new innovations or else refute the hypothesis and help Congress and HHS avoid mistaken policies in the future," the department argued.
De Liban countered that the waiver authority "isn't just a blank check to try out any idea [officials] might have no matter how perverse or harmful it will be to beneficiaries."
He noted that Health and Human Services Department approved Arkansas' waiver request without even having an estimate of the number of enrollees who would lose coverage.
Under the law, the approval of a waiver must be based on "reasoned analysis that considers all the relevant factors," De Liban said.
According to the San Francisco-based Kaiser Family Foundation, a health policy research organization, seven other states also have received federal approval to add work requirements to their Medicaid programs, including requirements that have taken effect in New Hampshire and Indiana.
Six other states have applied for approval to add similar requirements to their programs.
A Section on 04/13/2019