State Sen. David Sanders said Friday that he favors dropping the effort to create a state-run health insurance exchange for individual consumers unless more support emerges among other state leaders for making it part of the private option's overhaul.
RELATED ARTICLE
http://www.arkansas…">Governor sets private-option special session
The Little Rock Republican, one of the private option's legislative architects, has been a key backer of the effort to transfer operation of the insurance exchange from the federal government to the state.
Gov. Asa Hutchinson, who has proposed making changes to the private option and renaming it Arkansas Works, has said he doesn't see a need for a state-based exchange for individual consumers.
Sanders' declaration came as the state Department of Human Services released new figures on the number of Arkansans who have been approved for coverage under the state's expanded Medicaid program, known as the private option.
As of the end of January, 267,590 Arkansans had been approved for coverage under the program, according to the department. The total includes more than 18,000 state residents who were approved for coverage in December and January.
The number exceeds the 250,000 predicted by the Human Services Department, but the program's overall cost from July through December was about $101 million below the $814 million that a department consultant had projected for the first half of the fiscal year, department spokesman Amy Webb said.
For the entire fiscal year, which ends June 30, the department now expects the cost to be $74.7 million under the budgeted cost of $1.6 billion.
The state created the private option in 2013 as a primary way of extending Medicaid coverage to adults with incomes of up to 138 percent of the poverty level: $16,243 for an individual, for instance, or $33,465 for a family of four.
Under the program, the state Medicaid program buys coverage on the federally run health insurance exchange for the newly eligible adults.
The state received a $99.9 million federal grant to design a state-run exchange, and failing to follow through on the plan will require the state to return at least part of the grant.
Enrollment in a state-run exchange for small-business employees, established with money from the federal grant, started Nov. 1.
A state board's plans for an exchange for individual consumers, which would replace the federal exchange, had been put on hold while state officials consider changes to the private option and other parts of the Medicaid program.
Sanders said Friday that he had hoped the state would apply for a waiver from requirements under the 2010 Patient Protection and Affordable Care Act that would allow Arkansas more flexibility in designing the exchange.
"I am disappointed that that's at least not on the table in the first wave of discussions" between state and federal officials over a revamped private option, Sanders, R-Little Rock, said.
Hutchinson and other state officials visited with U.S. Secretary of Health and Human Services Sylvia Burwell on Feb. 1 to discuss the governor's proposed changes to the private option. A special legislative session will be held in April to determine how the program will be reshaped.
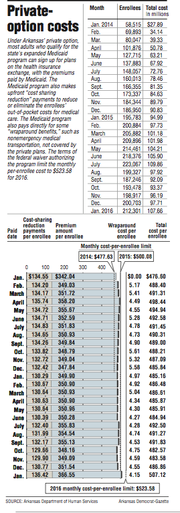
In addition to paying the premium for the individual insurance plans, the current private-option program provides additional subsidies, known as cost-sharing reduction payments, to cover the plans' deductibles as well as most or all of the enrollees' other required out-of-pocket spending for medical care.
It also pays directly for nonemergency medical transportation and other so-called wraparound benefits that are required under Medicaid rules but aren't covered by the insurance companies' plans.
According to the figures released by the state Department of Human Services on Friday, the average premium under the program rose in January by $15.02, to $366.55, reflecting premium increases for exchange plans that were approved for this year.
The average cost-sharing reduction payment rose by $5.64, to $136.42, while the average cost of wraparound benefits fell by 40 cents, to $4.15.
At $507.12, the per enrollee cost was below the target of $523.58 set in the federal wavier authorizing the private option.
The federal government is expected to pay the full cost of the expanded Medicaid program, including the private option, through the end of this year as long as the private option's cost per enrollee stays below a cap calculated by using the monthly targets.
In 2014, the first year of the program, the program's cost, adjusted for a rebate paid by one of the insurers, averaged $485.50 per enrollee -- more than $7 above the waiver's target of $477.63.
Last year, however, the average monthly cost per enrollee rose only slightly, to $486.98, while the cost target rose to $500.08.
From Jan. 1, 2014, through January 2015, the total cost was about $2 billion, about $23 million below the limit indicated by the monthly targets, the Human Services Department's figures show.
The 267,590 Arkansans covered as of Jan. 31 included 212,301 who had completed enrollment in private-option plans by Dec. 15 as well as 22,793 people who were assigned to the traditional fee-for-service Medicaid program because their health needs were considered exceptional.
Tens of thousands of others had been approved for coverage and were being covered under the traditional Medicaid program because they had not yet completed enrollment, a process that involves completing a questionnaire about the applicant's health and, in most cases, choosing or being assigned a plan.
Human Services Department spokesman Webb said the program experienced lower-than-expected costs for those in the traditional Medicaid program. The department now expects that cost to be about $129 million, about $153 million below the department consultant's estimate, she said.
As for the higher-than expected enrollment, Webb said that was likely because of a reduction in employers who offer job-based coverage. For instance, she noted that the Legislature in 2014 passed a law ending employer-sponsored health coverage for part-time school employees.
The director of the Department of Finance and Administration's Employee Benefits Division said in December 2014 that about 600 employees were expected to be affected when the law took effect last year
The state also has seen a drop in people gaining approval for coverage under the traditional Medicaid program after they qualify for federal disability benefits, Webb said.
Some people who would have otherwise applied for the benefits, with the primary aim of obtaining health coverage, are likely applying directly for coverage through the expanded Medicaid program without seeking the disability benefits, she said.
The number of enrollees likely will decrease at the end of March as a result of an ongoing review of the eligibility of people who have been enrolled for at least a year, she said.
Hutchinson said in a statement Friday that the high enrollment "proves our case that real reform is needed."
Among the changes he has proposed are requiring enrollees with incomes above the poverty level to pay premiums of $19 a month and subsidizing some enrollees' coverage through employer-based plans.
A legislative task force is expected to make a recommendation on the proposed changes next month. The full Legislature will then vote on the matter during a special session that Hutchinson has said he plans to call in April.
Sen. Jim Hendren, R-Sulphur Springs and the task force's chairman, said the higher-than expected enrollment raises concerns about the cost to the state when it begins paying a portion of the expanded Medicaid program's cost.
The state's share will start at 5 percent next year and increase every year until it reaches 10 percent in 2020.
The cost "is going to have to be closely monitored," Hendren said.
Arkansas Works is "a great starting point," he said, but he and other legislators would like to see more changes.
"I think it's still in a state of flux," Hendren said.
A Section on 02/20/2016